The coronavirus disease 2019 (COVID-19) pan-epidemic, resulting from infection with the 2019 novel coronavirus (2019-nCoV), also known as severe acute respiratory syndrome-coronavirus-2 (SARS-CoV-2), is currently the source of public health concern worldwide; however, treatment of this infection has been clinically challenging in many patients [1]. Importantly, 2019-nCoV is the third fatal coronavirus that has emerged in the past two decades, following SARS-CoV and the Middle East respiratory syndrome (MERS)-CoV [2]. The numbers of confirmed cases of COVID-19 infection and related deaths are still rising. As of 9 March 2020, there have been 80 754 confirmed cases and 3136 deaths in the mainland of China [3], corresponding to a total crude mortality of 3.88%. Because the mortality is higher (14.4%) in severely ill patients (the estimated percentage of severe patients is 27.1%; 4794 of 17 721) [3], treatment strategies are urgently needed [4].
Hypercytokinemia, also known as "cytokine storm,” is a frequently occurring feature of severe infections with SARS, MERS, H5N1 influenza, and H7N9 influenza; it is associated with disease severity and is a predictor of mortality [5,6]. Studies of SARS have shown that elevated levels of the cytokines/chemokines interleukin (IL)-1, IL-6, IL-8, IL-12, interferon (IFN)- , IFN-
, IFN- -induced protein 10 (IP-10), and monocyte chemoattractant protein-1 (MCP-1) are associated with inflammation and extensive damage in the lung [7]. Elevated levels of IFN-
-induced protein 10 (IP-10), and monocyte chemoattractant protein-1 (MCP-1) are associated with inflammation and extensive damage in the lung [7]. Elevated levels of IFN- , IL-15, IL-17, and tumor necrosis factor-α (TNF-α) are also features of MERS-CoV infection [8]. Similarly, serum levels of IFN-
, IL-15, IL-17, and tumor necrosis factor-α (TNF-α) are also features of MERS-CoV infection [8]. Similarly, serum levels of IFN- , IL-6, IL-8, IL-10, IP-10, MCP1, and monokine induced by IFN-
, IL-6, IL-8, IL-10, IP-10, MCP1, and monokine induced by IFN- (MIG) were higher in H5N1 influenza-infected patients than in healthy individuals [5]. Moreover, patients with H7N9 influenza infection had higher levels of 34 cytokines and chemokines, such as hepatocyte growth factor, IL-6, IL-18, IP-10, MCP-1, macrophage migration inhibitory factor, MIG, stem cell factor, and stem cell growth factor-β [6]; notably, most of these cytokines/chemokines are pro-inflammatory.
(MIG) were higher in H5N1 influenza-infected patients than in healthy individuals [5]. Moreover, patients with H7N9 influenza infection had higher levels of 34 cytokines and chemokines, such as hepatocyte growth factor, IL-6, IL-18, IP-10, MCP-1, macrophage migration inhibitory factor, MIG, stem cell factor, and stem cell growth factor-β [6]; notably, most of these cytokines/chemokines are pro-inflammatory.
A previous study revealed high levels of pro-inflammatory cytokines/chemokines (e.g., IL-2, IL-7, IL-10, granulocyte-colonystimulating factor (G-CSF), IP-10, MCP-1, macrophage inflammatory protein 1α (MIP1A), and TNF-α) in severely and critically ill patients with COVID-19 infection; furthermore, the presence of cytokine storm was correlated with disease severity [2]. Studies revealed that the lethality of coronavirus or influenza virus is related to the induction of an excessive and aberrant immune response associated with severe lung pathology, with frequently fatal consequences [2,6,9–11]. Therefore, curbing the overt inflammatory response induced by COVID-19 may be essential for reducing mortality among severely and critically ill patients with COVID19 infection [2,12,13]. However, clinical management of severe patients infected with SARS or MERS has revealed that corticosteroid therapy did not reduce mortality; in contrast, it led to delayed viral clearance [14,15]. In tertiary hospitals in Hubei Province, China, systemic corticosteroids were used to treat severely ill patients with COVID-19 infection who exhibited significant acute pulmonary progression in imaging examinations; however, limited experience has shown that this strategy does not result in significant improvement [13].
In patients with SARS-CoV-related acute respiratory distress syndrome, cytokine-storm-targeted therapy was recommended to treat severe pulmonary failure secondary to an excessive inflammatory response [16]. Some studies showed that cytokine/chemokine clearance was achieved using artificial-liver bloodpurification systems consisting of blood-purification modules, such as plasma exchange, plasma absorption, and/or hemo/plasma filtration [17,18]. An artificial-liver blood-purification system was used to treat patients with severe H7N9 influenza infection who had confirmed cytokine storm and rapidly deteriorating condition [18,19]. Positive results were demonstrated in terms of remarkably reducing the levels of 17 cytokines/chemokines: basic fibroblast growth factor (FGF), G-CSF, macrophage-colony-stimulating factor, IFN- , IL-1 receptor antagonist, IL-12p70, IL-17A, IL-1β, IL-2, IL-4, IL-5, IL-8, IL-9, platelet-derived growth factor-BB, regulated upon activation normal T cell expressed and secreted (RANTES), TNF-α, and vascular endothelial growth factor. These encouraging results were achieved after the first session of artificial-liver blood-purification therapy and were maintained thereafter [18].
, IL-1 receptor antagonist, IL-12p70, IL-17A, IL-1β, IL-2, IL-4, IL-5, IL-8, IL-9, platelet-derived growth factor-BB, regulated upon activation normal T cell expressed and secreted (RANTES), TNF-α, and vascular endothelial growth factor. These encouraging results were achieved after the first session of artificial-liver blood-purification therapy and were maintained thereafter [18].
The experience gained in the treatment of critically ill patients with H7N9 influenza infection and cytokine storm revealed the high efficacy of plasma-exchange modules in artificial-liver blood-purification systems, based on the extent of cytokine clearance [18]. This result is consistent with the ability of plasma exchange to clear large molecules from the blood [17,20]. However, when the treatment of critically ill patients with H7N9 influenza infection was limited in cytokine clearance to the use of a continuous veno-venous hemofiltration (CVVH) module, there was a slight increase in cytokine/chemokine levels [18]. This may have reflected the ability of the CVVH module to eliminate inflammatory cytokines at a clearance rate slower than that of cytokine release, as well as ineffective clearance of protein-bound cytokines by hemofiltration [17]. In addition to scavenging inflammatory mediators, the combination of plasma exchange and a CVVH module in an artificial-liver blood-purification system can improve the management of metabolic disorder, fluid overload, and cardiovascular dysfunction [18].
Given the demonstrated efficacy of cytokine-storm-targeted rescue therapy in severely and critically ill patients with influenza virus infections, artificial-liver blood purification may be effective for treating severely and critically ill patients with COVID-19 infection, by similarly targeting the cytokine storm (Fig. 1). The artificial-liver blood-purification system was applied in Zhejiang Province, China, and showed good prognosis in the treatment of severely or critically ill COVID-19 patients with cytokine storm [21].
《Fig. 1》
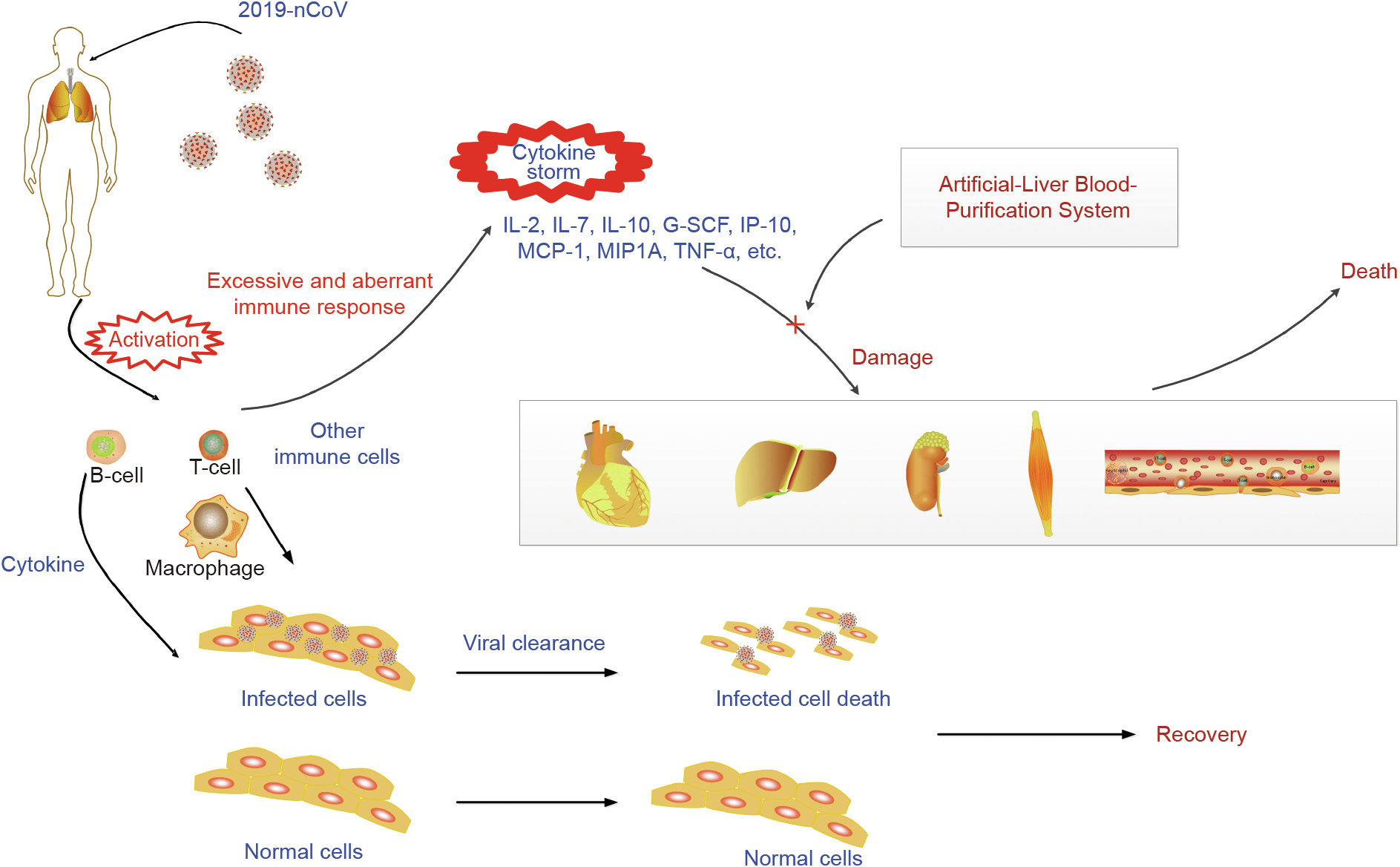
Fig. 1. The artificial-liver blood-purification system eliminates inflammatory cytokines/chemokines and alleviates cytokine-storm-induced damage in 2019-nCOV infection.
Based on the above-described evidence, the Expert Consensus on the Application of Artificial-Liver Blood-Purification System in the treatment of severe COVID-19 was recently released [22]. This work recommends artificial-liver blood purification for the treatment of patients with COVID-19 infection who exhibit cytokine storm and rapid disease progression, as confirmed by lung imaging. The similar recommendation was made in the Guide line for the Diagnosis and Treatment of COVID-19 (7th version) [23].
The Expert Consensus report [22] cites the following indications for artificial-liver blood-purification therapy in severely and critically ill patients with COVID-19 infection: ① a plasma concentration of blood inflammatory factors (such as IL-6) ≥ five-fold above the upper limit of normal, or a daily increase of > one-fold; ② rapid daily progression of lung involvement ≥ 10%, based on lung imaging, computed tomography, or X-ray; ③ comorbidities requiring artificial-liver blood-purification therapy.
It should be noted that conditions ① and ② must be met simultaneously, whereas condition ③ alone is sufficient for treatment implementation.
Further investigations may be conducted in the near future and should consider the following aspects: First, there is a need for multicenter clinical studies of anti-cytokine-storm targeted therapy for COVID-19 by novel artificial-liver blood-purification systems (i.e., Li’s artificial liver system (Li-ALS) [24]) with demonstrated abilities to clear pro-inflammatory cytokines (e.g., TNF-α, IL-1β, IL-2, IL-6, and IL-18). Second, investigations are needed regarding the key pathways and immune cell types involved in cytokine storm onset in COVID-19; these will benefit the understanding of artificial-liver support system treatment for alleviating cytokine storm to reverse the disease process in patients with severe COVID-19 infection by rebalancing the immune system. By acting as an anti-cytokine-storm targeted therapy, artificial-liver blood-purification systems hold excellent potential for reducing mortality in severely and critically ill patients with COVID-19 infection.
《Acknowledgements》
Acknowledgements
This work was supported by the grants from the Fundamental Research Funds for the Central Universities (2019FZA7001), the Mega-Project of National Science and Technology for the 13th Five-Year Plan of China (2017ZX10202202002001), and the National Natural Science Foundation of China (81600497).












 京公网安备 11010502051620号
京公网安备 11010502051620号