In its Top 10 Emerging Technologies report published in November 2020, the World Economic Forum—advised by experts convened by the journal Scientific American—placed ‘‘Microneedles for Painless Injections and Tests” at the head of its list [1]. It chose innovations to include ‘‘for their potential to spur progress in societies and economies by outperforming established ways of doing things” and their likely ‘‘major impact within the next three to five years,” despite not currently being in wide use.
To visualize a microneedle array patch (MAP), imagine a Band-AidTM, except swap its soft absorbent pad for a bristling patch of tiny, medicated barbs that can shallowly pierce the skin—painlessly (Figs. 1 and 2). By the end of this decade, such patches might start making the hypodermic needles routinely jabbed into your muscles today to inject vaccines and drugs a thing of the past. But that depends, in large measure, on whether biomedical and manufacturing engineers can achieve further advances beyond progress they have reported at recent medicaldevice meetings about developing production processes and equipment to mass-manufacture the small, but sophisticated gadgets.
《Fig. 1》

Fig. 1. (a) A Micron Biomedical MAP in protective shell prior to use (left). With coverings removed (right), it is ready to be turned over and applied to the skin by finger pressure. Credit: PATH, with permission. (b) When researchers in the laboratory of MAP pioneer Mark Prausnitz, professor of chemical and biomedical engineering at the Georgia Institute of Technology in Atlanta, GA, USA (also Micron Biomedical co-founder and chief scientific officer), fabricated this dissolving microneedle array, they mixed pink dye into the liquid polymer from which they molded the device. The colorant represents medically active ingredients such as vaccines or drugs that are incorporated into dissolving microneedles and released when interstitial fluid in the pierced skin wets and disintegrates the water-soluble projections. Credit: Georgia Institute of Technology, with permission.
《Fig. 2》

Fig. 2. (a) Peeling back the tab of a foil moisture-seal (right) from one end of the tablet-shaped package containing a Vaxxas high-density MAP (HD-MAP) reveals a springmounted, microneedle array (left) that is too dense for the relatively light, slow pressure from a finger to force the projections into the skin. Since this photo was taken, Vaxxas has switched to circular arrays as seen in Fig. 3. Credit: PATH, with permission. (b) Transdermal delivery of the dose of vaccine or medication coated on the array requires holding the open face of the canister against the skin and pressing down on the convex dome spring built into the lid. As the spring suddenly flips concave with a snap, it thrusts the array against the skin at 20 m·s–1 , fast enough to deny the skin time to deform and thereby punching the microneedles through the outermost skin layer. Credit: Vaxxas, with permission.
Less than a millimeter in length and numbering tens to thousands in an array typically small enough to be pushed into place with the tip of a finger, microneedles do not pierce the skin deeply enough to stimulate pain nerves. However, the lances still reach skin layers teeming with cells that vaccines can stimulate to martial immunity and with abundant blood and lymph circulation that can systemically deliver other medicines, all possibly more effectively than the standard shots now used for more than 150 years.
So far, however, no MAP has won the approval of national or international medical regulators. Nonetheless, since a few months into the pandemic in 2020, a consortium of organizations—Gavi (a Geneva, Switzerland-based funder of immunization programs, previously called the Global Alliance for Vaccines and Immunization), the World Health Organization, United Nations International Children’s Emergency Fund (UNICEF), PATH (a Seattle, WA, USAbased, global public health nonprofit, formerly called the Program for Appropriate Technology in Health), the Bill and Melinda Gates Foundation, and others—have redoubled efforts on multiple fronts to rigorously evaluate the technology and pave the way to realizing its potential benefits, in high-need, low-resource settings as well as everyday medical practice [2].
Since the first microneedle arrays were fabricated in silicon in the late 1990s with techniques developed for the electronics industry [3], researchers have studied them in the laboratory and in hundreds of animal model and clinical investigations. Trials testing MAPs containing vaccines and medications for dozens of different diseases have consistently demonstrated key advantages of the patches over needles and syringes. Not only do patients favor the pain-free experience of MAPs, but they generally can also safely and effectively administer MAPs to themselves, with the superficial skin damage from the microneedles posing minimal risk of infection [4,5]. Studies have shown that the potency of microneedle patches can endure lengthy shipping delays or storage, even at elevated temperatures and with little or no refrigeration [6]. Furthermore, in efficacy trials, relatively low vaccine doses from MAPs, when compared to intramuscular injections, often have provoked similarly robust immune reactions [7]. Those findings suggest, say vaccination experts, that the immunity MAP-administered vaccines can bestow might ultimately come at a significantly lower cost in terms of both side effects and expense.
The mounting evidence of these advantages has long stirred excitement in some quarters of the healthcare field, from biomedical device entrepreneurs to international public-health organizations. But now the challenges of coronavirus disease 2019 (COVID-19), the first global pandemic in a century, have illuminated in stark relief the downsides of needles, syringes, and multidose vials. Those include costly and cumbersome ‘‘cold-chain” requirements associated with liquid vaccines [8], the need for skilled personnel to administer them, and such perils as incorrect dosing, cross-contamination, and needle sticks, not to mention vaccine hesitancy due to fear of needles.
In July 2021, startup biotech company Micron Biomedical in Atlanta, GA, USA, launched the first clinical trial of vaccinating children with a MAP [9–11]. The trial lies at the leading edge of efforts organized by the coalition of global public-health and funding organizations to develop and commercialize the world’s first MAP vaccine—not for COVID-19, but for measles rubella (MR). Although children by the millions, particularly in developed nations, routinely receive vaccinations against this duo of pox diseases, the more virulent of the two—measles—remains a widespread and prolific killer of unvaccinated children in poor countries, accounting for an estimated 140 000 deaths in 2018 alone [12].
If the MR MAP project succeeds, ‘‘it will be a key pivot point from which to launch MAPs and accelerate them into the market, both for MR and for other applications,” said biomedical engineer Jessica Mistilis of PATH, a MR-project partner. Notwithstanding the global public-health community’s prioritization of MR, both commercial and academic labs are working on MAP vaccines for a range of other diseases as well, including COVID-19 [13–15].
The coalition’s MAP-based, MR vaccine development, funded by the Gates Foundation, focuses on two of the four main types of microneedle arrays [16]. The Micron Biomedical track uses the company’s dissolving microneedle arrays that are fabricated in molds from water-soluble polymer with the vaccine blended in. A parallel development track uses solid microneedles made from durable, injection-molded, vaccine-free plastic onto which a vaccine-rich layer gets deposited.
Dissolving microneedles begin to disintegrate as soon as they contact body fluids within the skin, releasing vaccine into the surrounding tissue. But only the coating of the solid microneedles melts away into the body. Vaxxas, a Brisbane, Australia-based MAP company makes the solid-microneedle array for the MR project. The company specializes in an exceptionally close-packed array containing up to 5000 microprojections per patch, called a high-density-MAP (HD-MAP), including a version under development to deliver a COVID-19 vaccine [17]. The remaining two major categories of MAPs include hollow microneedles with a typically laser-drilled conduit down the middle that delivers vaccines or drugs from a reservoir and hydrogel-forming microneedles that absorb water and release their immunologically or therapeutically active ingredients as they swell. The latter can control the release of water-soluble drugs from a reservoir atop the MAP at a rate set by the tightness of the gel’s mesh of polymer strands, said hydrogel microneedles’ inventor Ryan Donnelly, a professor in the School of Pharmacy at Queen’s University Belfast, in Northern Ireland. Comparing hydrogels for slow and fast release, ‘‘is almost like going between an onion bag and a soccer goal, in terms of the netting,” he said.
While regulatory approval for MAP products remains a significant obstacle, many of the technology’s developers and proponents see mass-manufacturing capabilities and capacity as the most urgent and difficult impediments to overcome. A study published in October 2021 by researchers at PATH of manufacturing readiness in the medical-microneedle-array field reports that no developers so far have created production-scale manufacturing facilities for their devices [5].
In 2020, Vaxxas announced that it would develop ‘‘the world’s first high-throughput, aseptic manufacturing line” for its MAPs. A German firm that specializes in pharmaceutical process lines and sterile manufacturing, Harro Höfliger in Allmersbach im Tal, is Vaxxas’s partner on the project [18]. Vaxxas chief executive officer David Hoey said that his company had begun preliminary mass-production-related design and fabrication with Harro Höfliger several years earlier.
At a virtual meeting in September 2021 of the International Society for Vaccines, Vaxxas publicly presented details and videos for the first time of progress to date on its prototype, HD-MAP production line (Fig. 3). Dispensing one drop of vaccine simultaneously onto all the microprojections of each newly formed MAP coming down the line allows a throughput of potentially millions of MAPs per week, Hoey said, with that goal emerging early as the company’s most critical and complex manufacturing engineering challenge.
《Fig. 3》

Fig. 3. A shallow cup holding a newly made microneedle array moves out from under the Vaxxas test-manufacturing system’s printhead (bottom right) after, in less than a millisecond, the printhead deposited nanoscale droplets simultaneously onto all the array’s approximately 5000 microneedles. Transported from the left toward the print head at the margins of a rotating platform, the arrays for HD-MAPs first undergo automated inspection by a camera mounted on the back of the vertical gray panel (left of center). The company is developing this pilot manufacturing line for sterile fabrication of up to 1 million HD-MAPs per week for Phase III clinical trials and early commercial production. The microneedles of each microarray seen on this pilot line occupy a circle whereas those of the Vaxxas HD-MAP shown in Fig. 2 form a square. The company has switched to the circular configuration which, when there is an angular discrepancy between the printhead and the array, requires less rotation—so less realignment time—thanks to the greater symmetry of the circular design. Credit: Vaxxas, with permission.
A video accompanying the conference talk shows a queue of newly formed microneedle arrays passing beneath a ‘‘printhead” of tightly packed, microfabricated dispensing nozzles precisely matching the arrays’ geometry and needle count [19]. As a camera-based visualization system measures the three dimensional orientation of each arriving array, the dispenser shifts, turns, and tilts itself to align with the microneedle tips. Every nozzle then—in unison—squirts a single 150-picoliter droplet on its target, after which the rapidly drying, coated array moves on to automated, optical and laser assays of coating thickness, consistency, and proper placement.
To prepare MAPs for earlier clinical trials, the first printhead that Vaxxas engineers developed passed its single nozzle sequentially over the microneedles in each row of what were then rectilinear arrays, shooting droplets onto the needles’ tips. By that method, ‘‘it took about 10 minutes to coat a patch,” Hoey said. ‘‘Where we need to be is 10 per second,” referring to the intended throughput of a pilot production line slated to begin operation in late 2024. Although the coating process reportedly operated at 200 MAPs per minute in the video—a third of the way to the target speed—the engineering currently in place is capable already of the faster pace the company is aiming for, he said.
‘‘The reproducibility of such tiny drops, controlling them to hit their targets, and ensuring they land where intended are the main challenges of coated needles,” said mechanical engineer Michael Kulik of LTS Lohmann Therapie-Systeme AG, an Andernach, Germany-based company. Daunting hurdles can turn up elsewhere in the production steps needed for different MAP types. As the world’s largest contract manufacturer of conventional transdermal drug delivery patches (no needles) for pharmaceutical-industry clients, LTS Lohmann is preparing to add MAPs to its business. Kulik leads development of the company’s manufacturing line for dissolving MAPs (d-MAPs).
During an early October 2021 presentation at the Microneedle & Transdermal Delivery Systems Virtual Summit 2021, Kulik showed videos of precision, robotic leveling, lifting, and placements of racks of liquid-polymer-laden molds within a dispensing module of the prototype production system (Fig. 4). Kulik also talked about a dilemma facing would-be manufacturers of all kinds of microarray patches, especially a contractor like LTS Lohmann. Because of the minimal risk of infection from MAPs compared to hypodermic needles and without clear guidance from regulators, many in the MAP field are asking: Must manufacturing lines be sterile (aseptic)? Or would it suffice to pay roughly half as much in capital costs to meet a less stringent, ‘‘low bioburden” standard? The price penalty looms especially large for agencies and organizations hoping to deploy vast numbers of MAPs in poor countries. Kulik said that for its prototype, d-MAP manufacturing system LTS Lohmann is creating a wide variety of equipment, capabilities, and processes. Clients may choose which to include in the production line among, for instance, assorted ways to optimally concentrate drugs or vaccines in microneedle tips or to satisfy regulatory requirements for low-bioburden or aseptic conditions.
《Fig. 4》
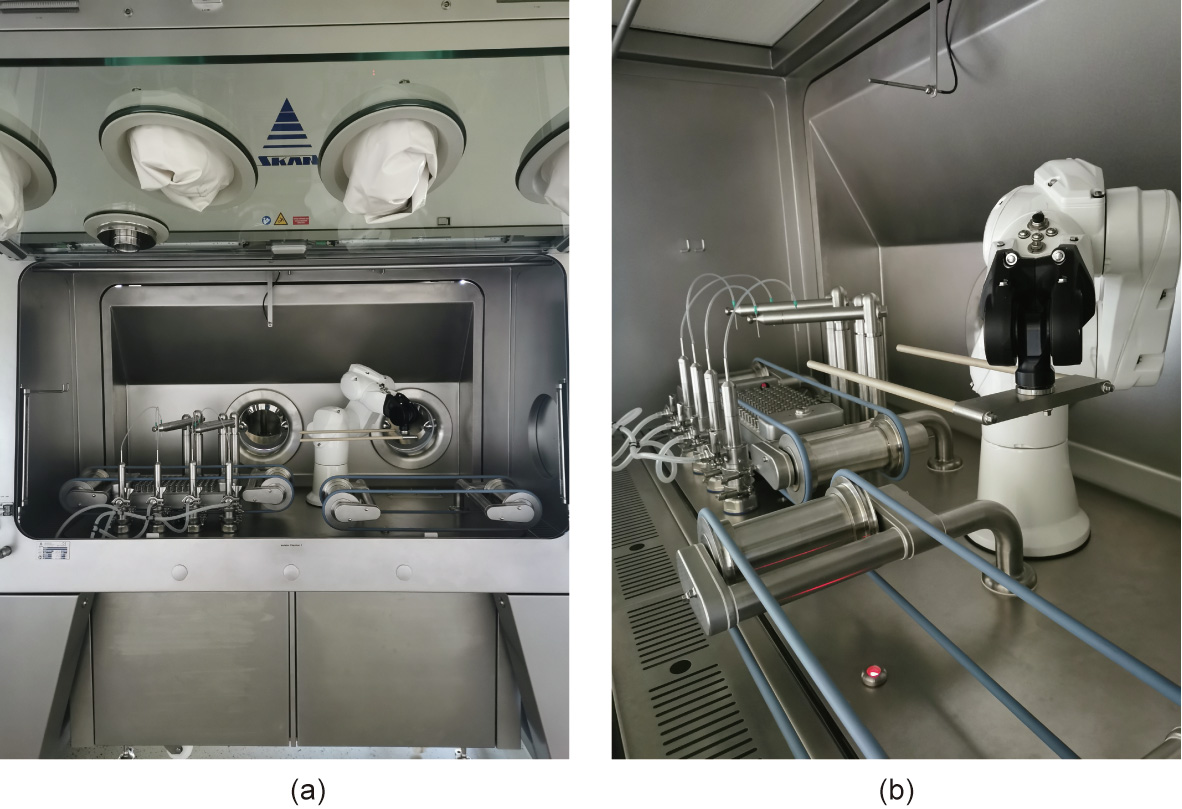
Fig. 4. (a) Flexible tubes and movable metal rods surround a robotic platform of a dispensing station to the left of a companion robot (right of center) in this prototype module of a d-MAP manufacturing line being developed by LTS Lohmann. The robotic platform can receive a rack (not shown) of empty microneedle-array molds from its fellow robot. The platform then deploys its rods to precisely raise portions of the rack to align the tops of all the molds to the same horizontal level, after which the tubes dispense liquid polymer blended with active pharmaceutical ingredients, such as a vaccine or medication, into the molds. The companion robot then lifts away each filled rack and sets a new, empty one in its place. LTS Lohmann has also built a prototype demolding and packaging module for the end of the line with the aim of fabricating one million d-MAPs per year on a pilot production system. Still in development are modules for distributing active ingredients selectively within filled array molds (by multiple means, such as centrifugation), and for the drying of filled molds. (b) Close-up views of the robotic dispensing station (rear), and companion robot (right) next to belts (front) that convey racks into and out of the module. Credit: LTS Lohmann, with permission.
Despite the barriers still in the way of widespread medical use of microneedle arrays, the field is active and growing (microneedle products for relatively unregulated cosmetic uses became commercially available years ago [20]). By November 2020, the number of medical MAP developers worldwide had reached nearly 90 [21]. In addition to the MR vaccine, developers are working on other projects within the Gavi alliance or sponsored by the US Biomedical Advance Research Development Authority, including MAP vaccines for rabies, polio, rotavirus, and flu, and MAP-based therapeutics for human immunodeficiency virus (HIV) and contraception [22]. Meanwhile, others are pursuing more novel applications in medicine and new twists on microneedle array technology. Sorrento Therapeutics in San Diego, CA, USA, innovates in both of those ways in its Sofusa Lymphatic Drug Delivery System, which is in clinical trials for diverse illnesses such as metastatic melanoma and rheumatoid arthritis [23,24]. Its MAP, with a drug reservoir, microfluidics, and microneedles with lengthwise grooves and other surface texture delivers large doses of drugs to the lymph nodes [13]. In June 2021, MAP developer TSRL in Ann Arbor, MI, USA, and biotech company PharmaTher, of Toronto, Canada, teamed up to develop therapeutic products based on hydrogel-forming MAP technology patented by Donnelly and colleagues that each company has independently licensed from Queen’s University Belfast. While TSRL intends to target flu and other viral diseases, PharmaTher’s work focuses on the treatment of mental illness and other disorders by means of MAP-delivered psychedelic drugs [25].
‘‘We are now at the point where drug makers think delivering substances across the skin could be worth a lot,” said Donnelly. ‘‘That could signal a step change where the pharmaceutical industry sees MAPs as more than just a technology for vaccines in the developing world.”












 京公网安备 11010502051620号
京公网安备 11010502051620号




