《1 Introduction》
1 Introduction
Public health emergency management is a series of actions, such as prior monitoring, early warning, emergency treatment, investigation, rescue, communication, accountability, prevention and preparation for public health emergencies, collaboration during the incident, and learning and improvement after the incident; it also involves emergency medical and rescue services which are implemented in other emergencies to reduce the danger of emergencies to global sociopolitical and economic systems as well as people’s lives [1]. The primary goal of public health emergency management is to prevent and reduce the occurrence of public health emergencies and to take measures to control the event to reduce possible impacts and losses.
A public health emergency system is the sum of a country’s vision, main players, institutional arrangements, and resource allocation in response to public health emergencies. In a health emergency system, the emergency command system plays a central role in emergency decision-making, and the success or failure of the command’s decisions is directly related to the success or failure of emergency work. After the severe acute respiratory syndrome (SARS) outbreak in 2003 and the influenza A (H1N1) outbreak in 2009, China actively explored the development of a public health emergency command system and established and continuously improved the mechanisms of joint prevention and control and expert advisory committees under the State Council. However, in the face of various major public health emergencies, China’s public health emergency command system still has many shortcomings and deficiencies. The global pandemic of coronavirus disease 2019 (COVID-19) has posed new challenges to China’s public health emergency command system.
《2 Evolution of China’s public health event emergency response system》
2 Evolution of China’s public health event emergency response system
《2.1 Basic features of China’s public health emergency system from the founding of the People’s Republic of China to the SARS outbreak in 2003》
2.1 Basic features of China’s public health emergency system from the founding of the People’s Republic of China to the SARS outbreak in 2003
The public health incident response system is an important component of the national emergency response system. After the establishment of the People’s Republic of China, all types of major emergencies occurred frequently and seriously threatened the safety of people’s lives, physical health, social stability, and national economic and property security. To respond to these major emergencies, China adopted a monolithic leadership system under the auspices of the State Council of the CPC Central Committee, mobilizing the military and soliciting the broad participation of society as a whole when necessary. As an integral part of the national emergency response system, China’s public health emergency management system has undergone different stages of development. Further, with the accumulation of experience in responding to public health events, the construction of China’s public health emergency management system has gradually moved toward normalization, specialization, and scientificization.
After the reform and opening up of the country in 1978, with the change in government functions and an increase in international cooperation, emergency management in China entered a new stage of development. In particular, after the SARS epidemic in 2003, China began a new chapter on the public health emergency system and capacity building. The SARS epidemic was a serious public health emergency that emerged in China at the beginning of the 21st century and prompted the modernization of China’s public health emergency response system.
From the founding of the People’s Republic of China to the early 1980s, the focus of China’s public health efforts was to establish a healthcare network based on a “prevention first” system. Urban communities, towns, and rural areas rely mainly on primary health centers, epidemic prevention stations, and rural doctors to provide basic medical and public health services. These primary care institutions and epidemic prevention stations are designed to provide basic medical and public health services in the region and are not equipped to respond to large-scale public health emergencies. In addition, the administration of this disease prevention and control network underwent restructuring several times: administrative and health care agencies merged during 1958–1961, and epidemic prevention agencies were reduced, abolished, and restored during 1967–1971. However, from the 1980s to 2003, with the influence of market-oriented reforms, the national health epidemic prevention system evolved into an organization that “emphasized clinical care over prevention, paid over unpaid services, and more revenue over less revenue” (1985– 2003) [2], which had an impact on the effectiveness of China’s health emergency response system.
《2.2 SARS promotes the construction of a health emergency response system with “one plan and three systems” as the basic framework》
2.2 SARS promotes the construction of a health emergency response system with “one plan and three systems” as the basic framework
The SARS epidemic in 2003 not only put forward requirements for the establishment of a sound disease prevention and control system in China but also pushed the country to start the systematic construction of a comprehensive emergency response system. After its victory against the SARS epidemic, China began to strengthen its national emergency response system with “one plan and three systems” as the core content [3]. Under this framework, the emergency management of public health emergencies in China began to institutionalize and normalize practices, and a comprehensive health emergency command system was gradually established.
In terms of laws and regulations, the State Council promulgated the Regulations on Emergency Response to Public Health Emergencies in 2003, which established a legal system for public health emergencies in four aspects: prevention and emergency preparedness, reporting and information dissemination, emergency response, and legal responsibility. In 2005, the Ministry of Health issued the National Information Reporting Management Standards for Public Health Emergencies (for trial implementation), which made clear provisions for the normalization and timely effectiveness of public health emergency monitoring. In 2006, the Ministry of Health issued the National Emergency Plan for Public Health Emergencies and the National Health Emergency Protection Plan for Public Emergencies, which clarified the emergency organization and protection systems for health emergency management.
In terms of system construction, in February 2007, the Ministry of Health further clarified that the overall goal of health emergency work during the Eleventh Five-Year Plan period is to establish a sound system of health emergency management laws and regulations and health emergency plans and to build an emergency management mechanism that is: “unified in command, responsive, coordinated and orderly, and operates at high speed.” By 2009, before the emergence of the H1N1 epidemic, 30 provincial health departments in China (in autonomous regions and municipalities directly under the central government’s leadership) had set up emergency response offices. The Chinese Centers for Disease Control and Prevention (CDC) and some provincial disease control centers had also set up specialized emergency response departments [4]. The organizational system of emergency commands for public health emergencies that had been established at that time is shown in Fig. 1.
《Fig. 1》
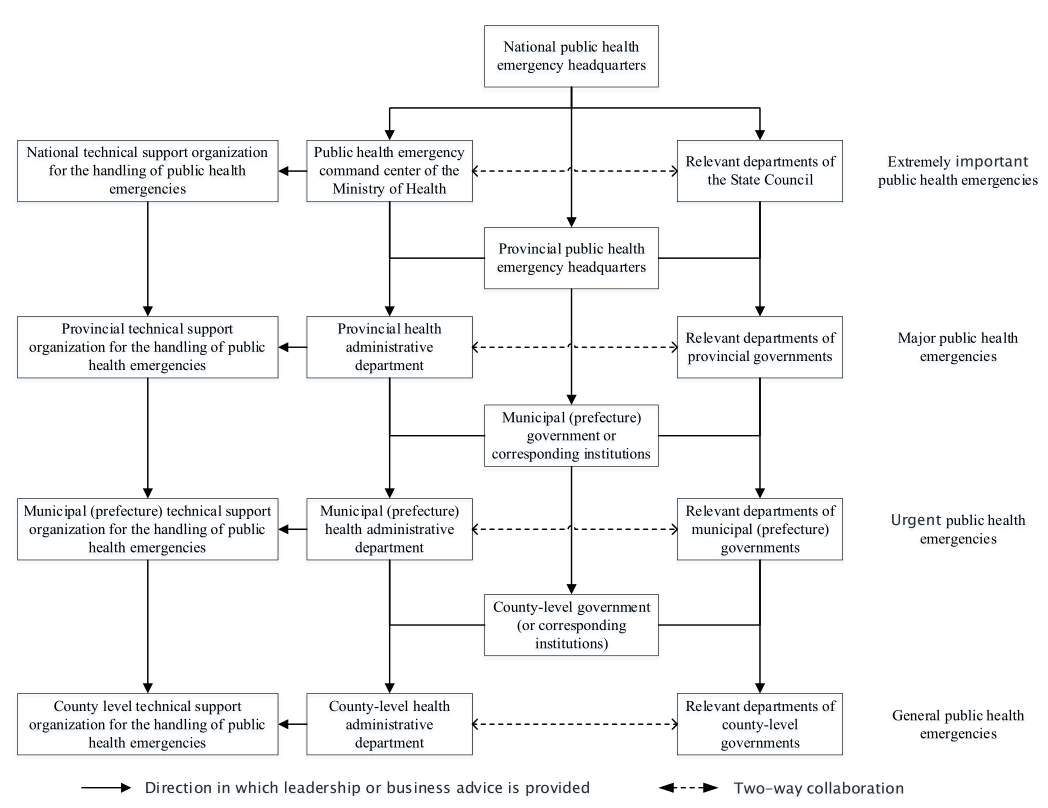
Fig. 1. Emergency command and organization system of public health emergencies in China (2009).
Note : The former Ministry of Health is now the National Health Commission.
In 2010, 2011, and 2012, respectively, the Ministry of Health issued documents such as Guidance on Accelerating the Construction and Development of Health Emergency Response System for Public Emergencies, Multi-departmental Emergency Response Coordination Mechanism for Public Health Emergencies, and Management Measures for Public Health Risk Assessment of Public Emergencies to guide health emergency work and improve public health emergency response capabilities. In terms of public health emergency response team construction, the National Health Emergency Work Standards for Medical Institutions (for trial implementation) and the National Health Emergency Work Standards for Disease Prevention and Control Institutions (for trial implementation) were released in 2015 and 2016, respectively. In addition to macrolevel public health emergency management policies, special policies related to the management of public health emergencies were introduced in China after SARS [5].
In terms of emergency command systems, the worldwide outbreak of H1N1 in 2009 prompted China’s public health emergency system to enter a new stage of development. The prevention and control of H1N1 in China was divided into six phases: prevention and preparation, early warning response, early-epidemic, mid-epidemic, lateepidemic, and late-pandemic [6]. In response to the major prevention and control command initiatives of H1N1, the country established an 8+1 joint prevention and control mechanism led by the Ministry of Health. Under this mechanism, there were eight working groups consisting of 33 departments (later expanded to 38 departments) and units: general, port, medical, security, publicity, foreign cooperation, science and technology, and animal husbandry and veterinary medicine. An expert committee on H1N1 prevention and control was also formed. Simultaneously, the working mechanism for joint prevention and control of H1N1 and the responsibilities and rules of procedure for each working group and expert committee were also clarified, and a meeting system for all members and liaison officers was established [6]. According to the regulations, the main responsibilities of the national joint prevention and control work mechanism were to regularly discuss and judge the development trend of the epidemic; study and determine prevention and control strategies; agree on policies, response plans, and major measures related to prevention and control work; coordinate and guide all relevant departments and regions to implement various prevention and control measures; and organize supervision and inspection of the implementation of prevention and control work [7]. The practice of H1N1 prevention and control provided valuable information to China about how to deal with subsequent epidemics, especially foreign epidemics.
《2.3 Development and application of joint prevention and control mechanisms for the response to public health emergencies》
2.3 Development and application of joint prevention and control mechanisms for the response to public health emergencies
In 2009, China began exploring the establishment of joint prevention and control mechanisms. Following the COVID-19 outbreak on January 20, 2020, the State Council continued the joint prevention and control model and initiated the joint prevention and control mechanism. The joint prevention and control mechanism is led by the National Health Commission, a multi-ministerial coordination working mechanism platform at the central government level, with an adjusted membership of 32 departments [8], as shown in Fig. 2. This is an emergency organization mechanism with a high administrative level that has played an active and effective role in containing the epidemic, helping infected patients, protecting the general population, and restoring social order.
《Fig. 2》

Fig. 2. Joint prevention and control mechanism of the State Council in response to COVID-19 in 2020.
In addition to the State Council’s joint prevention and control mechanism, China has also established a central leading group for an epidemic response to strengthen the unified leadership and command of national epidemic prevention and control. At the meeting of the Standing Committee of the Central Political Bureau held on January 25, 2020, a leading group was established to deal with the epidemic, working under the leadership of the Standing Committee of the Central Political Bureau [9].
Expert participation mechanisms are gradually becoming scientific and important in the Chinese health emergency command system. The Regulations on Emergency Response to Public Health Emergencies, promulgated in 2003, mentioned expert participation for the first time, and the National Emergency Response Plan for Public Health Emergencies, issued by the State Council in 2006, clarified the status and responsibilities of expert participation. The Strategy for Prevention and Control of Acute Infectious Disease Outbreaks, issued in 2007, further established the role of experts in command and coordination, early warning, and the talent pool. Therefore, in both H1N1 and COVID-19 epidemic prevention and control, experts played a role in policy-making, consulting, and technical support. At the same time, after nearly 20 years of the evolving public health emergency response practice, China also established support institutions and platforms, such as information centers and command platforms, to serve emergency decision-making.
《3 Challenges facing China’s public health emergency command system》
3 Challenges facing China’s public health emergency command system
《3.1 The current and future public health emergency situation is severe》
3.1 The current and future public health emergency situation is severe
The situation of public health emergencies in China is grim, and different types of events occur frequently and concurrently, such as the frequent occurrence of public health events, mainly infectious diseases; increased difficulty in preventing and controlling public health events caused by food and drug safety issues; and the increased risk of public health events caused by biotechnology misuse. These events resulted in multiple emergency command system responses at a complex level.
Since the beginning of the 21st century, new acute infectious diseases such as SARS, H5N1, H1N1, Middle East respiratory syndrome (MERS), H7N9, and COVID-19 have emerged in countries worldwide, while the occurrence and spread of infectious diseases such as Ebola hemorrhagic fever, dengue fever, and the plague remain very severe. According to the World Health Organization, infectious diseases accounted for three of the top 10 causes of death worldwide in 2019: lower respiratory infections, diarrheal diseases, and neonatal diseases (including neonatal sepsis and infections), with lower respiratory infections remaining the world’s deadliest infectious disease [10]. Therefore, both notifiable infectious diseases and outbreaks of acute infectious diseases, as well as infectious diseases imported from abroad, are public health emergencies in need of response. Food and drug safety issues, another category of a public health emergency, also occur occasionally. Although China has introduced a series of food and drug safety laws and regulations, the foundation in this area is still weak, and the resulting public health incidents are difficult to prevent and control. In recent years, incidents, such as gene editing and gene therapy abuse, have made biosafety issues more prominent. As global climate change, ecosystem imbalance, microbial evolution, increased globalization, accelerated population migration, and increased scope of human social activities all provide conditions for the occurrence of public health events, the risks and challenges of public health emergencies will become greater in the future.
《3.2 The existing public health emergency system has outstanding shortcomings》
3.2 The existing public health emergency system has outstanding shortcomings
In response to a particularly major outbreak of an acute infectious disease such as the COVID-19, China’s existing public health emergency response system has some obvious shortcomings and deficiencies, which in turn restrict the emergency command capability. First, although China’s current infectious disease reporting system is capable of rapid reporting, accurate surveillance and early warning capabilities are inadequate in the early stages of an outbreak. Second, the professional capacity of health emergency response teams varies worldwide, leading to low efficiency and a lack of orderly organization of health emergency responses in some places during serious epidemics. Third, in the early stages of an epidemic, medical emergency supply reserve management was irrational, mobilization and distribution efficiency was low, and resource sharing and emergency requisition compensation could not be achieved on time. Fourth, the release and dissemination of emergency information at the beginning of the epidemic was not timely and the application rate of science and technology innovation was relatively low. Fifth, the health emergency management capacity of some localities and cities is not strong enough, and in many areas, health emergency response capacities at the grassroots level are even lower because they lack professional management technicians. Sixth, public health institutions are not set up properly, and cohesion between the upper and lower levels and the division of responsibilities are not clear, resulting in poor communication between departments. Seventh, although the country has introduced a series of emergency management regulations and policies, there is not yet a unified and complete system of health emergency regulations and standards, resulting in a mixed structure.
The above-mentioned shortcomings and deficiencies of the public health emergency system will affect the capacity building of health emergency commands, especially the role of joint prevention and control mechanisms. Even if the joint prevention and control mechanisms can play a full role, the response to a serious outbreak of a particularly acute infectious disease, such as the coronavirus pneumonia outbreak, is not sufficiently robust, and a higher level of command and coordination decision-making is needed for follow-up.
《3.3 Lack of professional strength to respond to public health emergencies》
3.3 Lack of professional strength to respond to public health emergencies
The occurrence of SARS in 2003 pushed the national disease prevention and control system to progress significantly. Not only has hardware improved significantly, China has also built the world’s largest direct reporting system for infectious diseases and public health emergencies, both vertically (above the township level) and horizontally (all health institutions). However, since the reform and opening up of China, the institutional mechanism that emphasizes medical treatment over prevention has not been completely changed.
From 2008 to 2020, China’s disease prevention and control workforce remained under pressure, with a serious loss of top talent [2]. Additionally, the occurrence of H1N1 in 2009 did not do much to improve the predicament in which the disease prevention and control sector found itself; from 2010 to 2018, the total number of personnel in disease prevention and control centers at all levels in China decreased by 3.9%, including a 10.8% decrease in practicing physicians as the main professional and technical force, while the total number of personnel in general hospitals increased by 64.3% in the same period [11]. Disease prevention and control institutions’ share of healthcare expenditures decreased from 2.9% to 2.4% [12]. More importantly, the three-tier preventive healthcare network was replaced by a three-tier medical service network. In general, there was a tendency to deviate from the “prevention first” approach, both in terms of policy and configuration.
《3.4 International situations pose challenges to China’s public health emergency command system》
3.4 International situations pose challenges to China’s public health emergency command system
The COVID-19 pandemic has ushered in dramatic international changes. Due to the different policies, political situations, economic strengths, and cultures of each country, the consequences and impacts of the COVID-19 pandemic on all aspects of each country vary greatly. In addition to long-term permanent human damage, this global pandemic has had a negative impact on the global economy and geopolitical situations, which are difficult to estimate. Some countries have failed to respond effectively to the pandemic and have even politicized the fight against it, leading to a greater loss of human life and property.
Through this pandemic, we learned that the existing global health governance mechanism is far from meeting the needs of global public health. In a globalized society, the major public health events that China will face in the future will require a global perspective. The construction of China’s health emergency command system should not only consider the protection of national life and property but also consider how to play a proactive and leading role in an uncertain and unstable international environment. China should collaborate with other countries to play their respective strengths and establish a more orderly and effective collaborative response mechanism.
In summary, the risks posed by public health emergencies are inherently multiple and complex and their impact is significant. In-depth research and practical exploration are needed in a variety of areas: the relationship between sectoral professional decision-making and comprehensive political decision-making in public health emergency commands, vertical activation of emergency command organizations, horizontal emergency linkage mechanisms for different levels of public health emergencies, and how to play a leading role in guaranteeing the better use of experts, information, technology, and decision-making platforms. Furthermore, the emergency command of public health emergencies poses greater challenges to the leadership of decision makers, and leadership improvement training for health emergency decision-making commands should be given more attention. We need to continue to adhere to the general policy of “prevention first,” as much as possible, to achieve public health emergencies from reactive emergency response to active prevention.
《3.5 China’s public health emergency command system mechanism has shortcomings》
3.5 China’s public health emergency command system mechanism has shortcomings
First, the division between power and responsibility is not sufficiently clear. The emergency command system for the COVID-19 outbreak is a politically driven national emergency command system for major public health emergencies that rely on the advantages of the socialist system with Chinese characteristics, which emphasizes ad hoc centralized and unified leadership. This politically driven emergency command system is highly effective in the early response to a disease outbreak. However, as the COVID-19 pandemic has continued over a longer period, this system has not been clearly defined in terms of authority, responsibility, and benefit between departments, regions, and levels, leading to crossover cooperation challenges in practice. At the same time, too much emphasis on upward centralization of power tends to weaken the main consciousness, main role, and spirit of innovation and accountability of localities and departments, thus leading to a lack of responsiveness among individual localities and departments in the early stages of major public health emergencies.
Second, there was insufficient institutionalization and stability. The response to the COVID-19 outbreak, both at the central and local levels, was mainly an ad hoc task-oriented organization whose status and operating procedures were not entirely clear in the Emergency Response Law, Infectious Disease Prevention and Control Law, Emergency Regulations for Public Health Emergencies, and other laws and regulations and emergency plans. Simultaneously, the mechanism was activated with the occurrence of an epidemic and ended at the end of the epidemic, which was not conducive to accumulation and long-term stable development and led to various problems in the practical work process. For example, owing to the lack of standardized and specialized design of goal orientation, connotation, supporting institutions, operating mechanisms, and standards of the joint prevention and control mechanism, joint prevention and control sometimes remain at the discourse level and are prone to problems in implementation [13].
Third, the cost of prevention and control is relatively high, and the adjustment is not sufficiently fast. There are various types and levels of public health emergencies, and it is necessary to follow the principle of proportionality and insist on the lowest possible administrative cost and the least possible damage to the interests of the administrative counterparts to achieve effective control of the situation. In the face of the different developmental stages of an epidemic, preventive and control measures of corresponding strength need to be taken to achieve the organic synthesis and rapid conversion between “concentrated power for big things” and “decentralized power for small things” to reduce the cost of response as much as possible. China’s national emergency command system for major public health emergencies, which primarily relies on political tasks and means to achieve the integration and dispatch of various emergency forces and resources, was necessary and effective for a short period during the COVID-19 response. However, the organization is expensive and difficult to sustain in the long term. For example, China’s zero-tolerance model for COVID-19 cases has played a key role in breaking the chain of domestic transmission and keeping imported cases very low. However, as the pandemic perpetuates, new variants continue to emerge, and herd immunity, even achievable through vaccines, cannot fully eradicate the virus. This strategy faces the diminishing returns problem epidemiologically, politically, economically, and diplomatically.
Fourth, there is still a lack of clear and explicit rules/institutions or reasonable and smooth channels for professional departments and expert resources to participate in emergency health management and provide professional advice. For example, there are no specific rules designed for the selection of experts. The National Health Commission’s expert group for the prevention and control of the COVID-19 epidemic lacks the necessary interface with the existing National Expert Advisory Committee on Public Health Emergencies; the mechanisms for internal information sharing among expert group members and expert participation in outbreak discussions remain incomplete [14]. In the meantime, it remains necessary to further explore how to embed public health, disease prevention and control, and other professional agencies in the administrative system into the political authority-based command system.
《4 Policy recommendations for improving the comprehensive emergency command system for public health emergencies in China》
4 Policy recommendations for improving the comprehensive emergency command system for public health emergencies in China
《4.1 Improving the joint prevention and control mechanism in accordance with the law and regulations》
4.1 Improving the joint prevention and control mechanism in accordance with the law and regulations
On one hand, there is an urgent need to enhance the legal status of the joint prevention and control mechanism and to clarify its specific status in the legal hierarchy at all levels. In the current legal hierarchy in China, that is, the Constitution (fundamental law), laws (basic and general laws), administrative regulations, local regulations, departmental regulations, and local government regulations, the lower-ranking legal formulation has a law to follow. It is necessary to clarify the specific status, functional positioning, structural composition, and operational mechanism of the joint prevention and control mechanism in the existing emergency laws and regulations, emergency plans, and related policy texts in China, especially to improve its due rank in the legal rank and to strengthen the legal status and authority of the joint prevention and control mechanism. On the other hand, the provisions of laws and regulations should be refined, experience and inadequacies should be summed up, and grassroots frontline urban and rural community joint prevention and control mechanisms should be improved and refined in the presence of ambiguous management rights and responsibilities. To strengthen the institutionalization of joint prevention and control mechanisms, we need to summarize the potential effects of the mechanisms and consequences of human error and poor operations. Further, there are several issues in need of refinement at the grassroots level, such as the management of “gray areas” and “multiple management” in institutional settings, power and responsibility configuration, and composition of personnel. In this way, we might avoid politicizing everything, overshooting, frictional conversion between peacetime and wartime, or implementation distortion problems.
《4.2 Strengthening the laws and standards for emergency status, warning classification, emergency command, and response classification》
4.2 Strengthening the laws and standards for emergency status, warning classification, emergency command, and response classification
On the one hand, there is a need to clarify the specific criteria and management system of the Emergency Regulations for Public Health Emergencies, the National Emergency Plan for Public Health Emergencies, and other emergency plans regarding the grading of early warning and emergency response. The differences and connections between the two must be determined, and the workflow from early warning to emergency response must be better connected. However, there is an urgent need to further establish the authority of relevant government departments in emergency situations, normalize the procedures related to policy formulation and adjustment of government departments' emergency responses, and develop standardized and normalized workflows. At the same time, there is an urgent need to revise the provisions of the Prevention and Control of Infectious Diseases Law regarding the identification and adjustment of infectious diseases and to revise and supplement the Emergency Response Law for deficiencies and gaps in the prevention and control tests of the coronavirus pneumonia outbreak to provide adequate legal protection for the prevention and control of major outbreaks.
《4.3 Establishing institutionalized channels for expert consultation and support on public health emergencies》
4.3 Establishing institutionalized channels for expert consultation and support on public health emergencies
On one hand, China should establish a national expert pool for public health emergencies and systematically consider the selection of experts, mechanism designs of the complementarity of expertise, and prior coordination among different experts. Simultaneously, the country should take the initiative to strengthen cooperation with the World Health Organization and relevant international organizations to include top international experts in expert consultation. On the other hand, the State Council should take the lead in establishing an expert mechanism to enhance the depth and breadth of expert consultations on public health emergencies. At present, the members of the expert advisory committee in the joint prevention and control mechanism include not only experts in the field of healthcare but also experts in economic and social management. The potential role of the expert advisory committee has not been fully utilized due to insufficient participation and the lack of a continuous and stable working mechanism. Therefore, establishing specific mechanisms to promote the depth and breadth of expert consultation is the key to the next step. The government’s role should be to provide relevant information to experts and clarify the mechanism of expert responsibility to avoid excessive administrative intervention.
《4.4 Clarifying the central- and local-level emergency command authority and responsibility》
4.4 Clarifying the central- and local-level emergency command authority and responsibility
In establishing emergency organizations and command systems, the central-level emergency organization and command system should focus on mobilization and coordination, allowing the local level to assume more specific decision-making and command functions. In response to public health emergencies, the central government should take the lead in coordinating the resources of all parties and in making decisions on major issues of principle and overall importance. At the same time, local governments would be allowed to establish appropriate emergency commands and comprehensive coordination agencies in accordance with the spirit of the policies formulated by the central government, which would consider the actual local situation and shift the decision-making power on specific issues to the frontline. The joint prevention and control mechanism of the COVID-19 outbreak response fine-tunes the working methods under the existing emergency management system and has proven to be a positive reference for future public health emergency management practices.
《4.5 Command mechanism construction should pay more attention to domestic and foreign collaborations》
4.5 Command mechanism construction should pay more attention to domestic and foreign collaborations
In the context of globalization, countries around the world are highly interconnected, and this trend is irreversible. In the face of major public health security challenges, no country can detach itself from the interconnected world, and it is necessary to actively collaborate with the World Health Organization and UN agencies to strengthen global public health through international exchanges and cooperation. Therefore, China should specifically consider the following bilateral and multilateral forms of international cooperation: (1) cooperating with the World Health Organization and relevant UN agencies to promote the reform and improvement of the existing global health governance system; (2) establishing exchange mechanisms with related countries to communicate the lessons learned in responding to public health emergencies, to support the capacity building of less-developed countries and countries participating in the Belt and Road Initiative in response to the threat of infectious diseases; (3) establishing coordinating and data-sharing platforms dedicated to addressing global public health emergencies; and (4) establishing a global public health education, research, and talent network.
《Acknowledgments》
Acknowledgments
We thank Liu Xi, Li Beixi, Wu Yue, and Ji Shuwei of Tsinghua University for their contribution to this study.













 京公网安备 11010502051620号
京公网安备 11010502051620号




