《1. Introduction》
1. Introduction
According to the Public Health Agency of Canada’s Economic Burden of Illness in Canada report, cardiovascular disease-related physician care, hospital care, and drugs cost 11.7 billion Canadian dollar in 2008, and was the largest burden on the health system [1]. Likewise, cardiovascular disease is the leading cause of morbidity and mortality worldwide, and significantly impacts quality of life [2]. Currently, there is no cure for key cardiovascular diseases such as myocardial infarction (MI) and arrhythmia, as the heart has a very limited innate capacity for repair. Available therapies such as pharmacological interventions, coronary artery bypass graft surgery, and ventricular assistant devices have significantly improved patients’ quality of life and prolonged their longevity [3−5]. However, new therapeutic interventions with lower cost and higher efficacy are still required for the future.
The use of regenerative medicine to treat cardiovascular diseases has emerged as a research topic in the past few decades. Furthermore, recent advances in genomics and molecular medicine have brought the concept of personalized treatment for cardiovascular disease to the fore [6]. The advent of human-induced pluripotent stem cells (iPSCs) opens a new chapter for regenerative medicine because they are a potential cardiomyocyte source [7]. Indeed, human iPSC-derived cardiomyocytes have been engineered into cell sheets, which significantly improved cardiac function when implanted into infarcted rat hearts [8]. iPSC-derived cardiomyocytes have also been used to study cardiac ion channel pathology and arrhythmia pathogenesis mechanisms in vitro [9]. However, the limited survivability of implanted stem cells remains a major obstacle to cardiac regeneration.
Bioengineering has the capacity to alleviate this problem. Biomaterials can be delivered alone, or serve as a scaffold or carrier for cells or growth factors [10−12]. The therapeutic potential of both natural and synthetic biomaterials has been demonstrated in animal models of MI and peripheral artery disease (PAD) [13]. Specifically, the application of injectable biomaterials results in decreased left ventricular wall dilatation, increased angiogenesis, enhanced endogenous tissue repair via endogenous stem cell recruitment, and the preservation of cardiac function [12,14].
In this review, we focus on cardiovascular diseases that induce conduction abnormalities and their current interventions; biomaterial types that have been investigated in cardiovascular research; and the potential of these biomaterials for future therapeutic intervention. Since current research focuses largely on improving cardiac function and cardiac tissue regeneration, relatively little has been done in terms of evaluating conductive polymer potential for correcting cardiac event-related arrhythmias and conduction block in vivo. We thus specifically explore the potential of conductive polymers to correct arrhythmias and improve conductivity in the infarcted heart. Future challenges in translating conductive polymer work from bench to bedside will be examined as well.
《2. Regenerating the injured heart》
2. Regenerating the injured heart
《2.1. Cell therapy treatment of ischemic heart disease》
2.1. Cell therapy treatment of ischemic heart disease
Coronary artery disease (CAD) is the most common type of heart disease and the leading cause of death around the world [2]. Coronary arteries supply oxygenated blood and nutrients to the heart muscle. CAD is caused by the deposition of cholesterol-containing plaques in the arterial wall, resulting in vessel wall-thickening and narrowing of the vascular lumen. The narrowing of coronary arteries leads to decreased blood flow and causes cardiomyocyte ischemic injury. Patients with decreased blood flow to the heart experience chest pain (angina), shortness of breath, and limited exercise capacity. A complete blockage of the vessel causes MI, leading to cell necrosis and massive loss of cardiomyocytes [15]. The current standard intervention for ischemic heart disease centers around lifestyle modification, pharmacological interventions, and surgical interventions [16]. Patients who do not respond well to all available treatments may progressively develop heart failure, which requires a heart transplant.
Cell therapy (in which cellular material is injected into animals or patients) has emerged as a potential strategy for treating MI. Multiple candidate cell types have been proposed and investigated, such as bone marrow mononuclear cells [17,18], embryonic stem cells [19,20], skeletal myoblasts [21,22], endothelial progenitor cells [23], and cardiac stem cells [24,25]. Although improved cardiac function was observed in both animal and human studies [26−28], several obstacles remain, such as low cell retention/engraftment, cell delivery efficiency, electromechanical integration, and long-term safety [29−33]. Improving these elements is critical for future cell therapy research. Biomaterials may be the answer, as they serve as excellent scaffolds for cell delivery and tissue engineering. Cells can be either mixed with biomaterials and delivered to the injured site directly or cultured on biomaterial-based scaffolds for future transplantation [34,35].
《2.2. Biomaterials in cardiac repair and regeneration》
2.2. Biomaterials in cardiac repair and regeneration
In order for biomaterials to be feasible for cardiac repair, they must be biocompatible, be biodegradable, reduce local microenvironment hostility, persist for a sufficient time period to facilitate cell engraftment and integration with native tissue, and act as a reservoir for the slow release of bioactive molecules [36−38]. Both natural (gelatin [39], collagen [40], alginate [41,42], chitosan [43], and fibrin glue [44]) and synthetic (poly(lactic- co-glycolic acid) or PLGA [45], carbon nanotubes [46], and polyurethane [47]) biomaterials have been investigated as candidates for cardiac regeneration [37].
《2.3. Natural biomaterials》
2.3. Natural biomaterials
A biomaterial can be introduced to the heart as an injectable hydrogel or a patch [48]. Collagen, a major component of the extracellular matrix (ECM), is one of the popular natural materials used in cardiac repair. Miyagi et al. [10] investigated the effect of a collagen patch as a slow-release reservoir of the vascular endothelial growth factor (VEGF)-165 to promote vascularization in a right ventricle defect rat model. They found that the collagen patch with immobilized VEGF enhanced the growth of endothelial and bone marrow cells in vitro. A VEGF-collagen patch, when implanted onto a defective right ventricular free wall of the heart, resulted in elevated angiogenesis and ventricular wall thickness when compared with a control collagen-only patch. These findings indicate that growth factor immobilization onto a collagen patch improves cardiac repair via the promotion of cell recruitment and proliferation [10]. A collagen patch alone has been shown to preserve infarcted heart contractility, attenuate adverse remodeling, and improve heart function. It did this by diminishing infarct region fibrosis, supporting blood vessel formation between the infarct region and the patch, and attracting various native cells (e.g., smooth muscle cells, epicardial cells, and immature cardiomyocytes) to populate the patch [49]. Collagen is also used as a cell carrier to deliver various cell types to infarct regions after infarction. Frederick et al. [50] have shown that vitronectin/collagen scaffold seeded with endothelial progenitor cells induced neovasculogenesis and preserved ventricular function post-MI in a rat.
Chitosan is the second most abundant polysaccharide in nature, and has been widely used in agriculture, food and nutrition, environmental protection, and material sciences [51]. The chitosan gel has a porous sponge structure [52], and can be used as a cell scaffold [53] or carrier for controlled and localized drug delivery [54]. Liu et al. [43] have shown that an injectable chitosan hydrogel enhanced stem cell engraftment and survival by improving oxidative stress in the ischemic heart through reactive oxygen species scavenging and chemokine recruitment. A chitosan-collagen hydrogel has also been used to deliver an angiopoietin-1 analogue to enhance endothelial cell function and survival. Indeed, the angiopoietin-1 analogue-bound hydrogel mitigated endothelial cell apoptosis and stimulated endothelial cell tube-like structure formation [55]. Finally, implantation of a chitosan-hyaluronan/silk fibroin patch in an infarcted rat left ventricle (LV) resulted in reduced LV dilatation, increased wall thickness, and improved heart function [56].
Aside from collagen and chitosan, other natural biomaterials have also been investigated as candidates for cardiac regeneration therapy. Alginate is a polysaccharide derived from seaweed [57] and has been extensively investigated in wound healing, drug delivery, and tissue engineering [58]. Research investigating the effect of alginate implantation in MI models has shown that an injectable aliginate-hydrogel injected into the myocardium can be completely absorbed and replaced by connective tissue within 6 weeks. It was effective in reinforcing scar thickness, attenuating adverse ventricular dilatation, and improving cardiac function, whether injected 7 days or 60 days after MI [41]. These results could be a useful reference for administration timing in future studies. The peri-infarct zone injection of an alginate-chitosan hydrogel was also shown to be effective in preventing LV remodeling and promoting tissue repair by reducing cell apoptosis and increasing angiogenesis in an acute MI rat model [59]. Fibrin glue, which is primarily made of fibrinogen and thrombin, is used to create a fibrin clot. It is usually used to repair left ventricular wall rupture secondary to acute MI. The glue can seal the ruptured myocardium immediately and be naturally absorbed [60−62]. Christman et al. [44] investigated the effect of fibrin glue scaffold implantation on cardiac function preservation post-MI. Scaffold implantation resulted in the preservation of infarct wall thickness and cardiac function 5 weeks after injection in a rat model of ischemia-reperfusion injury [44].
《2.4. Synthetic biomaterials》
2.4. Synthetic biomaterials
Synthetic biomaterials are generally constructed from synthetic polymers, metals, or a combination of both. Synthetic biomaterials possess excellent strength and durability, but present increased toxicity, creating biocompatibility issues [48]. Like their natural counterparts, synthetic biomaterials are generated and used with the aim of serving as a reservoir for gradual and controlled drug delivery, and acting as a scaffold to support cell engraftment and integration.
Polylactic acid (PLA), poly-glycolide (PLG), and their copolymer PLGA are commonly used synthetic materials. Mukherjee et al. [63] employed a nanostructured matrix made of poly( L-lactic acid), poly( ε-caprolactone), and collagen to mimic the native microenvironment of the myocardium. A nanoscale PLA-co-poly( ε-caprolactone)/collagen biocomposite scaffold was used to culture and support isolated rabbit cardiomyocytes. The results showed that adult rabbit cardiomyocytes attached to the scaffold exhibited growth and cell organization comparable to that found in native myocardium [63]. Insulin-like growth factor (IGF)-1 bound to PLGA nanoparticles was delivered to the peri-infarcted area immediately after MI. The results showed that IGF-1-complexed PLGA nanoparticles prolonged IGF-1 retention in the tissue, reduced cardiomyocyte apoptosis, and improved LV function [45].
Carbon nanofibers have also been investigated for cardiac engineering. Martins et al. [64] mixed conductive carbon nanotubes with chitosan to form a chitosan/carbon scaffold with similar elastic properties to native myocardium. This conductive scaffold not only supported neonatal rat cardiomyocytes survival in vitro, but also increased the expression of myosin heavy chain, troponin T, and connexin-43, which are involved in muscle contraction and electrical coupling and are important for the organization of cell-cell electrical signal transmission [64]. Zhou et al. [65] also developed a carbon nanofiber/gelatin hydrogel scaffold that supported in vitro culture of neonatal rat cardiac cells and integrated with the host myocardium when implanted post-MI in the rat heart. Heart function as assessed by fractional shortening and ejection fraction evaluated by echocardiography was improved after hydrogel injection while progression of pathological deterioration (e.g., ventricular dilation) was inhibited [65].
Synthetic peptide-based biomaterials have also been investigated. Synthetic peptides are able to self-assemble into three-dimensional (3D) hydrogels with adjustable fiber dimensional properties and potential nanoscaling [66]. They can be directly injected into myocardium to improve the microenvironment for cell recruitment and survival [67], but also can act as a carriers for drug and cell delivery [68]. Tokunaga et al. [69] used the self-assembling peptide Puramatrix to deliver cardiac progenitor cells into border-zone myocardium after MI to ensure effective cell delivery and improve cell survival. In addition, self-assembling peptide nanofibers were used to deliver platelet-derived growth factor (PDGF) in a sustained manner in order to protect cardiomyocytes from apoptosis and preserve cardiac function post-MI [70].
Polyurethane, a durable and flexible synthetic polymer, was synthesized into an elastomeric patterned film to match the physical and mechanical properties of native cardiac tissue and investigated as a scaffold for tissue engineering. Cardiomyocytes seeded on patterned polyurethane film were able to grow following the film pattern and form a multilayered contractile tissue construct [71].
Despite the fact that clinical trials examining the application of biomaterial to cardiac diseases are scarce, a recent clinical study did report the clinical outcomes following 6 months of follow-up [72]. The authors found that alginate-hydrogel in addition to standard medical therapy (SMT) for patients with advanced chronic heart failure (HF) was more effective than SMT alone for improving exercise capacity and symptoms. The results from a year of extended follow-up for this clinical trial were also recently reported [73]. It was shown that alginate-hydrogel in addition to SMT was more effective than SMT alone for providing sustained 1-year benefits in exercise capacity, symptoms, and clinical status for patients with advanced HF. These data support further larger clinical evaluations of this novel therapy.
《3. Conduction abnormalities and arrhythmia》
3. Conduction abnormalities and arrhythmia
《3.1. Ventricular arrhythmias》
3.1. Ventricular arrhythmias
MI is often associated with increased incidence of arrhythmias, particularly ventricular arrhythmias [74,75]. Due to the limited regenerative ability of the heart, massive loss of cardiomyocytes post-MI leads to the formation of scar tissue, which is primarily composed of fibroblasts and collagen. Scar tissue has significantly decreased contractility and electrical signal conduction, leading to the formation of abnormal conduction pathways and the development of conduction block. Ventricular arrhythmias, either ventricular tachycardia (VT) or ventricular fibrillation (VF), are very common in MI patients, and are the major cause of sudden cardiac death (SCD) [76]. In acute MI, the ischemic cardiomyocytes in and around the infarct zone have altered electrophysiological properties, which serve as a potential risk for developing re-entrant loop (a circular electrical pathway), a mechanism for sustaining ventricular arrhythmias. As the MI passes the acute phase and the scar starts to stabilize, the scar tissue actually serves as an anatomical block promoting the development of re-entrant loop, which is a trigger for SCD [76]. Although medical interventions significantly decrease morbidity and mortality, SCD accounts for 70% of deaths of outpatients with CAD and more than 50% of deaths in the total patient population [77,78]. Dyssynchronized contraction (a difference in the timing, or lack of synchrony, of ventricular contraction in the heart) resulting from VF leads to decreased hemodynamics, circulatory collapse, and the loss of cerebral function.
Current therapies for ventricular arrhythmias are based on an established understanding of arrhythmia triggers, such as electrolyte imbalance [79], anatomical changes, ischemia [74], hypoxia [80], and physical and mental exertion [81]. The primary goal of current therapy is to restore normal heart rhythm. Immediate defibrillation and cardioversion is required for VF or pulseless sustained VT. The early administration of β-blockers (drugs designed to stabilize cell membranes and minimize the overall metabolic demands of the heart) is associated with a reduced incidence of VF [82,83]. Another clinical intervention is the use of an implantable cardioverter defibrillator (ICD), an electrical device designed to stop fibrillation and restore normal rhythm, which has been routinely used in patients with cardiomyopathy and survivors of sudden cardiac arrest (SCA) [78,84]. Despite the clinical use of ICDs for terminating arrhythmias in patients, VT or VF can still occur, and are associated with increased mortality and HF risk [85].
《3.2. Atrioventricular (AV) block》
3.2. Atrioventricular (AV) block
Heart rate and cardiac contraction is controlled by the sinoatrial (SA) node located in the right atrial wall, which is a natural pacemaker that generates and sends electrical impulses through the atria. This signal is then slowed by the atrioventricular (AV) node, located in the inferior posterior region of the interatrial septum, before reaching the ventricles to allow for complete atrial contraction. The impulse then reaches the ventricles via the bundle of His, which branches into right and left bundle branches and terminates in the Purkinje fiber system, facilitating synchronized ventricular contraction [86]. An abnormality in any of these components will cause a conduction disorder, which affects the pumping function of the heart [87].
AV block is a conduction disease that occurs when the electrical signal from the atria is partially or completely blocked by the AV node so that ventricular rhythm is decreased. Conditions such as neuromuscular disorders (e.g., muscular dystrophy) [88,89], systemic diseases (e.g., cardiac sarcoidosis [90] and amyloidosis [91]), myocardial ischemia/infarction [92,93], neoplastic disorders (e.g., primary cardiac lymphoma [94]), and catheter ablation [95,96] can all cause abnormal AV conduction [86]. Disruption of electrical signal conduction can occur at the AV node and at the infra- or supra-AV node structures, as well as at the bundle of His and the bifurcation of the left and right bundle [97−100]. The consequence is that the atrial electrical impulse is either delayed or only partially propagated to the ventricles, which potentially results in HF and SCD if untreated [101].
Currently employed treatments for AV block vary depending on the etiology and symptomatology. While asymptomatic AV block requires no intervention, symptomatic AV block (either innate or exacerbated during exercise) is treated with pacemaker implantation [100,101]. Indeed, permanent cardiac pacing is recommended in patients with AV block unless there is a reversible cause of AV block or a contraindication for pacemaker implantation [101].
Improving cardiac function and controlling arrhythmias are equally important. The efficacy of current therapies is limited by the different disease presentation of patients [102]. Therefore, new therapies are required to terminate abnormal conduction pathways and improve patients’ survival. Conduction disorders, such as AV block and ventricular arrhythmias, may benefit from conductive biomaterials−polymers that exhibit high electrical conduction. Preliminary investigations have already revealed that conductive biomaterials have great potential for improving conduction abnormalities induced by ischemic heart diseases and conduction block.
《3.3. Conductive biomaterials》
3.3. Conductive biomaterials
Polyacetylene, an organic conductive polymer, was first discovered and described in 1977 by Alan J. Heeger, Alan G. MacDiarmid, and Hideki Shirakawa. This discovery was recognized by the Nobel Prize in 2000 [103]. Conductive polymers are appealing not only because they exhibit electrical properties, but also because they are easy to synthesize, and are also biocompatible and biodegradable [104]. Conductive polymers have been used successfully as materials for biosensors, neural implants, drug delivery devices, and tissue-engineering scaffolds [105]. The conductivity of these polymers comes from their unique structure: a conjugated backbone formed by a series of alternating single and double bonds. These alternating bonds allow electrons to move freely between and within the chains [106]. The ability of conductive polymers to promote the generation of electrically active tissues, such as nerve tissue and heart tissue, has also been investigated [107,108].
There are many conductive polymers, such as polypyrrole (PPy), polyaniline (PANI), poly(3,4-ethylenedioxythiophene) (PEDT, PEDOT), polyazulene (PAz), and polythiophene derivatives [105]. Of these, PPy is one of the better-characterized polymers, having been extensively investigated in neuroscience and cardiac research.
George et al. [109] generated a PPy-containing conductive implant designed for neural prosthetics to guide neural stem cell (NSC) differentiation and neurite elongation. They found that PPy-containing conductive implants promoted the growth of neurons and glial cells around the implant when sutured in a rat cerebral cortex [109]. A conductive laminin/PPy film was able to guide human embryonic stem cells into neural lineages for nerve regeneration and repair [110]. In addition, PPy mixed with the counter-ion of dodecylbenzenesulfonate (DBS) was found to support the survival of NSCs and guide NSC differentiation toward neural lineages [111].
Potential applications for PPy in cardiac research have also been investigated. Kai et al. [112] created a nanofibrous membrane, composed of PPy, poly( ε-caprolactone), and gelatin, designed to mimic the ECM, for cardiac tissue engineering. They demonstrated that this membrane promoted human cardiac myocyte attachment, proliferation, interaction, and expression of cardiac-specific proteins [112]. A 3D PPy-coated PLGA polymer scaffold has been generated for potential stem cell transplant after MI. This conductive polymer scaffold is biocompatible, supporting the growth and proliferation of both cardiac progenitor cells and iPSCs. In addition, the PPy-coated PLGA scaffold could be electrically stimulated to modulate cell behavior [113]. PPy has also been shown to stimulate angiogenesis post-MI. Mihardja et al. [114] generated an alginate-PPy polymer and injected it into the infarct area, where increased angiogenesis was observed compared with saline-treated animals 5 weeks post-injection. In addition, myofibroblast infiltration was also increased in the infarct area [114].
To summarize, PPy conductive polymers not only provide suitable ECM support for cardiac cells, but also affect the biological behavior of cells. In tissue engineering combined with cell therapy, a conductive polymer-based cardiac tissue construct could be implanted in the heart post-MI to facilitate electrical signal conduction and integrate implanted cells with host cells.
Another potential application of conductive polymers is as a biological pacemaker. Patients with conduction block or HF are treated by the implantation of an electronic pacemaker, which controls heart rhythm and contraction in order to maintain heart pumping function [115]. Although such devices have shown potential in reducing mortality and hospitalization of patients, the fundamental problem−conduction block−is not yet solved because non-conductive tissue or an abnormal conductive pathway still exists in the heart. Research interest in developing a biological pacemaker began two decades ago in response to challenges and limitations facing electronic pacemakers, such as battery changes, chronic infection, high surgical cost, and device adaptation in developing pediatric patients (e.g., chest and vascular size, child growth, and congenital heart defects) [116−118]. In a normal heart, the SA node is the trigger that sends an electrical signal to the substrate−cells that sense and receive this signal. A trigger-substrate connection is critical for organized pacing and conduction. A biological pacemaker would be able to integrate with the heart, and respond to endogenous stimuli calling for increased/decreased cardiac activity [119]. In addition, implantation of a biological pacemaker would be minimally invasive, which is suitable for patients who have contraindications for electronic pacemakers [116]. Biomaterials play a role in biological pacemaker research by establishing communications between implanted pacemaker cells and their substrate cells, integrating implanted cells, and labeling and tracking transplanted cells in vivo [120−122]. Conductive polymers, as excellent biomaterial candidates, can act as an ECM to support cell survival while establishing electrical connections between cells (Fig. 1). As such, the development of a conductive polymer-pacemaker cell combination has great potential to be the first step in creating a biological pacemaker to be used in future therapeutics.
《Fig. 1》
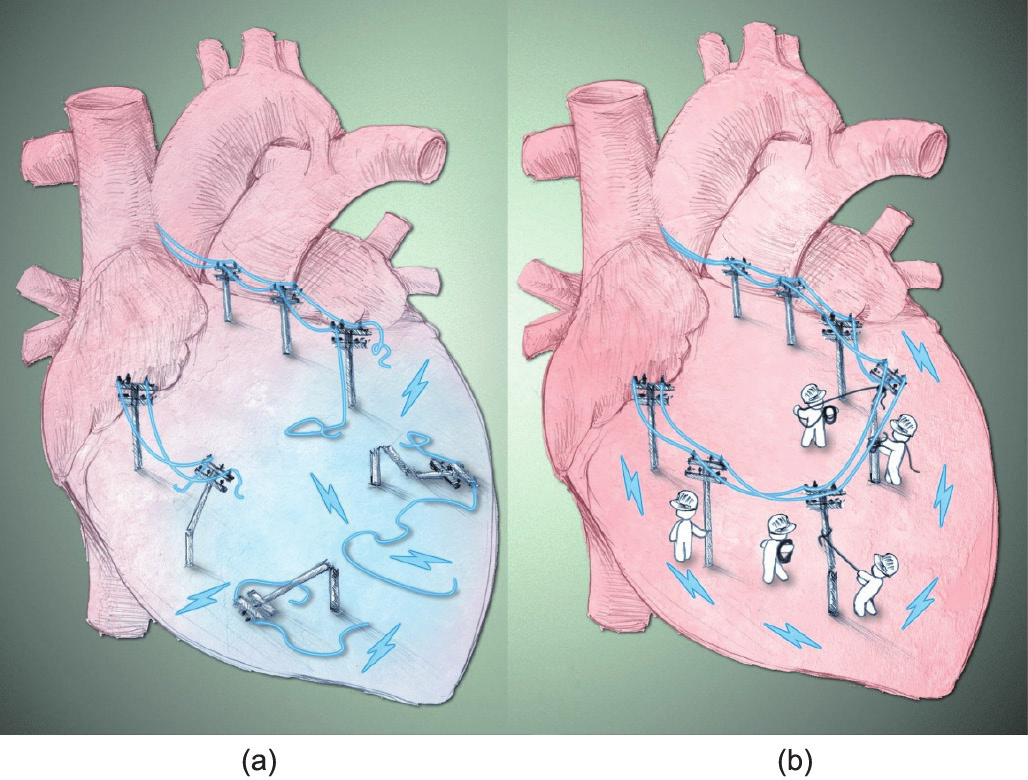
Fig.1 Reconnecting disrupted electrical signals in the infarcted heart. (a) Myocardial infarction induces a massive loss of cardiomyocytes, leading to scar tissue formation. Scar tissue disrupts electrical signal propagation, predisposing patients to increased risk of arrhythmia development. (b) The introduction of conductive polymers can reconnect damaged areas with existing healthy myocardium, thus repairing disrupted electrical conduction.
《4. Future challenges and directions》
4. Future challenges and directions
Biomaterials have great potential in cardiac repair and regeneration. The biocompatibility and biodegradation rate of most available biomaterials have been tested in different approaches by different groups. The future of biomaterials and tissue engineering is moving toward finding the ideal biomaterial-cell type combination for tissue regeneration. Selection of optimal cell types/combinations is vital for the success of tissue engineering, as the heart is a carefully balanced milieu of cardiomyocytes, fibroblasts, endothelial cells, and smooth muscle cells. Many questions remain to be answered. The major concern of biomaterial application to cardiac disease is the possibility of creating a substrate for arrhythmia. Although there are few studies that specifically address this risk, a recent study did reveal that the degree of the electrophysiological changes depends on the spread characteristics of the biomaterials [123]. This study found that hearts injected with highly spread biomaterials showed no conduction abnormalities. However, the injection of a biomaterial exhibiting minimal interstitial spread may create a substrate for arrhythmia shortly after injection by causing LV activation delays and reducing gap junction density at the site of the injection. This work demonstrates that the site of delivery and interstitial spread characteristics are important factors in biomaterial application-associated arrhythmias. In addition, generating biomaterials with elastic and strength properties similar to the native myocardium is critical [124]. Minimizing the immune response to prevent the encapsulation of biomaterials or tissue constructs is another concern, as encapsulation prevents proper integration of transplanted cells with the native environment [125]. Since the heart is the largest bioelectrical source in the body [126], synthesizing conductive polymers, which may facilitate the synchronous beating of cardiomyocytes, will enhance communications between transplanted tissue constructs and the native myocardium. This will be critical, as electrical field stimulation increases protein organization, facilitates cell polarization, and enhances electrical signal propagation [107]. Finally, the optimal timing for introducing biomaterials or tissue constructs remains unclear, and is vital for potentially minimizing inflammatory responses while limiting scar tissue formation.
Despite these challenges, biomaterial and tissue-engineering research holds great promise and has achieved much progress within the past two decades. The ultimate goal is to use biomaterial scaffolds in combination with appropriate cell types for partial or whole organ (re)generation. This will ultimately reduce the need for organ transplant, correct currently irreversible pathologies, and improve quality of life.
《Acknowledgements》
Acknowledgements
The authors thank Dr. Leigh Botly for help with manuscript preparation and editing. The illustration shown in Fig. 1 was conceived by Prof. Ren-Ke Li, with image art created by Benjamin Pakuts, Research Communications Officer at the University Health Network. This work was supported by a grant from the Heart and Stroke Foundation of Ontario (No. G140005765) to Ren-Ke Li. Ren-Ke Li holds a Canada Research Chair in cardiac regeneration. This work was also supported by a generous contribution by Eileen Mercier.
《Compliance with ethics guidelines》
Compliance with ethics guidelines
Zhi Cui, Baofeng Yang, and Ren-Ke Li declare that they have no conflict of interest or financial conflicts to disclose.













 京公网安备 11010502051620号
京公网安备 11010502051620号