《1. Introduction》
1. Introduction
Polycystic ovary syndrome (PCOS) is one of the most common endocrine disorders in women, affecting 5%–10% of women of reproductive age. PCOS is characterized by the three main phenotypes of hyperandrogenism, ovulatory dysfunction, and polycystic ovaries on ultrasonography [1]. Although the etiology of PCOS is still unclear, most experts consider it to be a multifactorial disease. Gonadotropic derangements, insulin resistance, hyperinsulinemia, adipose tissue dysfunction, and hyperandrogenism likely play important roles in the mechanisms of PCOS pathophysiology [2], and genetic/ethnic variation, mood disturbances, and lifestyle and environmental factors have also been suggested to be closely related to the etiology of PCOS [3]. The phenotypic diversity of PCOS can be affected by ethnic origin, geographic location, and even cultural and social practices [4]. Compared with European and North American women with PCOS, women with PCOS in Asia are generally shorter with a lower body mass index (BMI) and a milder hyperandrogenic phenotype, but greater menstrual irregularities [5].
Although there are 56 distinct ethnic groups in China, the Chinese Han make up 92% of the Chinese population [6], and there is thus little variation in genetic, racial, or ethnic characteristics among Chinese women. The territory of China lies between the latitudes 18°N and 54°N, and this vast geographic region is conventionally divided into northern and southern areas along the Qinling–Huaihe Line, which roughly follows the Qinling Mountains and the Huaihe River. The climate in Northern and Southern China varies significantly, so investigations that include geographic distribution might assist in understanding the effect of lifestyle and environmental factors on the epidemiology and phenotype of PCOS.
In recent years, obesity has become epidemic throughout the world due to an increased sedentary lifestyle and changes in diet [7], and obesity is especially common among women with PCOS. There is a growing body of evidence indicating that obesity negatively affects fertility and obstetric outcomes in women, including an increased risk of miscarriage and a higher risk of maternal and neonatal complications [8,9]. A recent randomized trial showed that intensive dietary and lifestyle interventions resulted in significant weight loss but did not substantially affect live birth rates in obese women scheduled for in vitro fertilization (IVF) [9].
The current paper summarizes the baseline characteristics of 1000 PCOS subjects and presents the effects of BMI and geographic distribution on the phenotypic features and clinical outcomes of clomiphene and acupuncture interventions.
《2. Material and methods》
2. Material and methods
《2.1. Setting》
2.1. Setting
Acupuncture and Clomiphene for Infertility in Polycystic Ovary Syndrome (PCOSAct) was a large-sample, multicenter randomized controlled trial for infertility among Chinese women with PCOS that took place from July 2012 to October 2015. It was the largest hospital-based PCOS study to date. Women with PCOS in this trial came from 21 sites (27 hospitals) almost all areas of the country and were generally representative of women with PCOS in China. A detailed protocol of the trial and the primary paper have previously been published [10,11]. The clinical trial identification is NCT01573858.
《2.2. Study population》
2.2. Study population
The study sample consisted of 1000 women who were diagnosed with PCOS according to the modified Rotterdam criteria [12], which are consistent with the Chinese PCOS criteria of the Chinese Medical Association [13]: oligomenorrhea or amenorrhea, together with clinical or biochemical hyperandrogenism. Other indispensable inclusion criteria included: aged between 20 and 40 years; at least one patent tube and a normal uterine cavity; husband sperm concentration ≥ 1.5 107 mL-1 and total motility ≥ 40%, or a total motile sperm count ≥ 10 million in the semen analysis; and agreement from the couple to have regular intercourse (2–3 times per week) during the study period.
《2.3. Interventions》
2.3. Interventions
The enrolled women were randomized into four groups: One group received clomiphene and active acupuncture, a second group received a placebo and active acupuncture, a third received clomiphene and control acupuncture, and a fourth received a placebo and control acupuncture. Clomiphene or a placebo was taken from day 3 to day 7 in every cycle, starting with an initial dose of 50 mg (1 tablet) and increasing to 150 mg (3 tablets) based on the treatment response. If the patient had a poor response, the dose would be increased by an additional tablet in the next cycle. The participants received active acupuncture or control acupuncture treatment twice a week, and each treatment session lasted for 30 min. Needles were placed at acupuncture points in the active acupuncture group, and needles were inserted at nonacupuncture points in the control acupuncture group. The treatment cycle lasted for four months. All treatments were stopped upon a positive pregnancy test. If the patient did not conceive, all measurements were repeated on the third day of menstruation in an ovulatory cycle, or within one week after the last acupuncture treatment in an anovulatory cycle. Once the patient was pregnant, treatments were stopped and the end-of study visit was performed within one week.
《2.4. Variables》
2.4. Variables
Clinical outcomes were ovulation, conception, pregnancy, live birth, and pregnancy loss. The outcomes of all pregnancies, including live birth, were followed after delivery or the termination of gestation [14]. Comprehensive biometric, historic, ultrasound, lifestyle, and questionnaire data were collected from all subjects at baseline. We also obtained the age, smoking history, and alcohol history from most of the male partners. Biometric information included height, weight, waist circumference, hip circumference, blood pressure, pulse, respiration, acne, hirsutism, and acanthosis nigricans. All patients’ medical histories included general history, pregnancy history, infertility treatment history, and family medical history. Research assistants who performed the physical examinations and obtained the patient history information at the local sites were trained and tested by international experts.
Reproductive and metabolic hormones were also measured at baseline. Blood was drawn on day 3 of menstruation, and all blood samples were stored frozen at the local site and then transported on dry ice to the central laboratory at the Heilongjiang University of Chinese Medicine every three months. The laboratory has ISO 15189 accreditation. Reproductive hormones included progesterone (P), luteinizing hormone (LH), follicle-stimulating hormone (FSH), estradiol (E2), testosterone (T), and sex hormone-binding globulin (SHBG). Metabolic indexes included insulin, glucose, high-density lipoprotein (HDL), low-density lipoprotein (LDL), cholesterol, triacylglycerol (TG), apoprotein A (APOA), and apoprotein B (APOB). The free androgen index (FAI) was calculated from measurable values for total T and SHBG using the following equation: FAI = (total T in nmol∙L-1 )/(SHBG in nmol∙L-1 ) 100. The homeostasis model assessment of insulin resistance (HOMA-IR) was obtained from the following calculation: HOMA-IR = (glucose in mmol∙L-1 ) (insulin in milliunit∙L-1 )/22.5. Metabolic syndrome was diagnosed using waist circumference, triglycerides, HDL, blood pressure, and fasting glucose [12] and was defined by meeting any three of the following five criteria: ① a waist circumference greater than 88 cm; ② a triglyceride level greater than 150 mg∙dL-1 ; ③ an HDL level lower than 50 mg∙dL-1 ; ④ systolic blood pressure greater than 130 mmHg (1 mmHg ≈ 133.322 Pa) or diastolic blood pressure greater than 85 mmHg; and ⑤ a fasting glucose level of 110–126 mg∙dL-1 . We defined normal weight as BMI < 24, overweight as 24 ≤ BMI < 28, and obesity as BMI ≥ 28 in Chinese women [15]. All BMI measurements are in kg∙m-2 .
《2.5. Data analysis》
2.5. Data analysis
In this study, all data entries were completed at the local sites. Data management, data auditing, and data analysis were performed in the Harbin project office under the supervision of the Data Coordination Committee for Statistics in Science at Yale University. Data were compared between treatment group, BMI categories, and by geographic distribution in Northern and Southern China. For categorical variables, we present the frequency and percentage in each group. For continuous variables, we present the mean and standard deviation in each group. Statistical significance was determined using Student’s t-test or the Kruskal–Wallis H test for continuous variables and the chi-square test or Fisher’s exact test for categorical variables. Differences were considered significant at P < 0.05. All analyses were performed with SAS version 9.4.
《2.6. Ethics》
2.6. Ethics
The protocol was approved by the local ethics committees at all sites, and all women signed a consent form before being enrolled in the trial.
《3. Results》
3. Results
Baseline demographics and clinical characteristics of the 1000 subjects are shown in Table 1. Patients were on average about 28 years old with a BMI of 24.2. The rates of hirsutism and acne were 26.6% and 32.4%, respectively. Acanthosis nigricans occurred in 18.5% of the women, 22.2% of the women had severe menstrual irregularities (amenorrhea), and 91.7% of the women had polycystic ovary morphology (PCOM). The average age of the male partners was approximately 30 years old, with an average sperm concentration of 9.74 × 107 mL-1.
《Table 1》
Table 1 Baseline characteristics by treatment arm.


The values in parentheses are total numbers or percentages.
WHR: waist-to-hip ratio; PCOM: polycystic ovary morphology; SBP: systolic blood pressure; DBP: diastolic blood pressure; CC: clomiphene citrate.
In terms of medical history, 7.2% of the women had a diagnosis of fatty liver in the past. The most common medical condition in the family histories of the women was diabetes mellitus (19.6%). A total of 50.2% of the women had a prior pregnancy but, among these, only 5.7% had live births. The average time spent attempting to conceive was 24.0 months. The numbers of women who were previously exposed to the study interventions were relatively low (29.4% for clomiphene and 12.4% for acupuncture). Of all the women, 13.8% exercised every day, 17.9% exercised every week, 20.7% exercised 1–3 times every month, and 47.7% did not engage in any regular exercise. Detailed serum profiles by treatment arms are listed in the primary paper [11].
With increasing BMI, menstrual irregularities and acanthosis nigricans were more serious; blood pressure, free T, FAI, insulin, glucose, HOMA-IR, LDL, cholesterol, TG, APOB, and lipoprotein levels were higher; HDL, APOA, E2, SHBG, LH, and LH/FSH levels were lower; and the incidence of metabolic syndrome was increased (Table 2).
《Table 2》
Table 2 Main characteristics by BMI categories.


The values in parentheses are total numbers or percentages.
MAP: mean arterial pressure.
SI conversion factors: To convert LH and FSH to IU∙L-1 , multiply by 1.0; P to nmol∙L-1 , multiply by 3.18; E2 to pmol∙L-1 , multiply by 3.671; total T to nmol∙L-1 , multiply by 0.0347; SHBG to nmol∙L-1 , multiply by 8.896; free T to nmol∙L-1 , multiply by 0.0000347; glucose to mmol∙L-1 , multiply by 0.0555; insulin to pmol∙L-1 , multiply by 6.945; triglycerides to mmol∙L-1 , multiply by 0.0113; and total cholesterol, HDL-C, and LDL-C to mmol∙L-1 , multiply by 0.0259.
a The Kruskal–Wallis test was used to compare the differences between the three groups.
Regarding the clinical outcomes between different BMI groups, the therapeutic effect was negatively correlated with BMI (Table 3). For normal, overweight, and obese women, the respective rates of ovulation per woman were 83.0%, 78.2%, and 63.6% (P < 0.001); the rates of ovulation per treatment cycle were 52.6%, 47.9%, and 36.6% (P < 0.001); the rates of conception were 34.6%, 32.4%, and 23.9% (P = 0.028); the rates of pregnancy were 25.1%, 19.1%, and 16.5% (P = 0.023); and the rates of live birth were 23.6%, 18.1%, and 15.3%, (P = 0.030). Pregnancy loss rates were comparable in all three BMI groups (P > 0.05).
《Table 3》
Table 3 Clinical outcomes by BMI categories.

Abs. diff.: absolute difference; CI: confidence interval.
a Live birth was defined as the delivery of a live-born infant ≥ 20 weeks’ gestation. Conception was defined as any positive serum level of human chorionic gonadotropin. Pregnancy was defined as an intrauterine pregnancy with fetal heart motion as determined by ultrasonography. Ovulation was defined as a serum progesterone level according to the standard of the local site laboratory (minimum value of luteal phase). Biochemical factor was defined as a positive urine or serum human chorionic gonadotropin test, but no fetus or gestational sac was visible on ultrasound.
b The chi-square test was used to compare the difference between three groups.
Women with PCOS in Northern China exhibited a higher BMI and waist-to-hip ratio (WHR) compared with women with PCOS in Southern China (25.4 vs 23.0 and 0.88 vs 0.86, respectively) and more severe acne (Table 4). Furthermore, Northern Chinese women with PCOS were associated with worse metabolic parameters, including higher glucose, HOMA-IR, APOB, and TG levels and lower HDL levels. More women in Northern China had a general history of fatty liver and a family history of hypertension, genital system neoplasms, and pregnancy complications. Southern Chinese women with PCOS exercised more often, and more women with PCOS in Southern China had previously received clomiphene and acupuncture therapies than women with PCOS in Northern China. Women with PCOS in Northern China had lower rates of ovulation per woman compared with women with PCOS in Southern China (74.8% vs 81.2%, absolute difference 6.4% (95% confidence interval (CI) 1.2%–11.5%) and risk ratio 0.9 (95% CI 0.9–1.0), P = 0.015) (Table 5), while rates of live birth, conception, pregnancy, and pregnancy loss were comparable with those of women with PCOS in Southern China.
《Table 4》
Table 4 Main characteristics by geographic distribution.
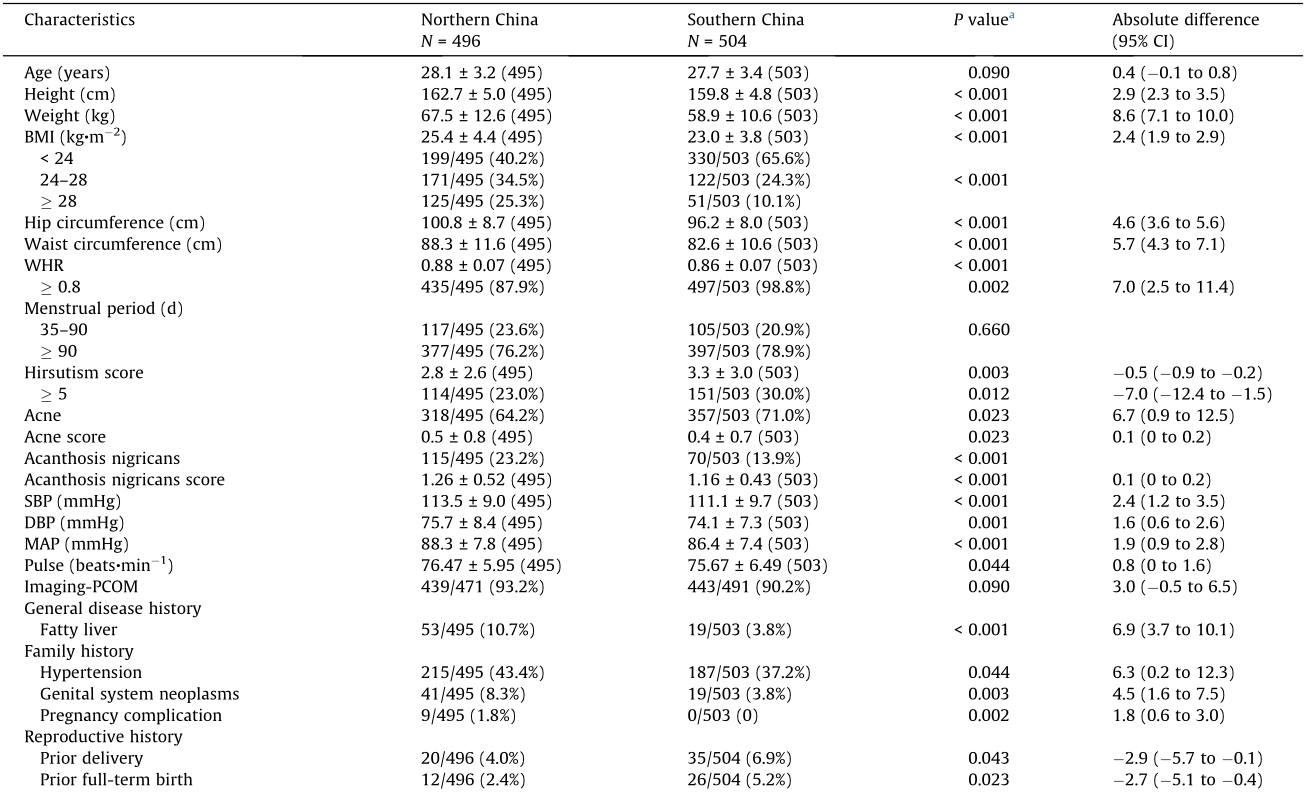
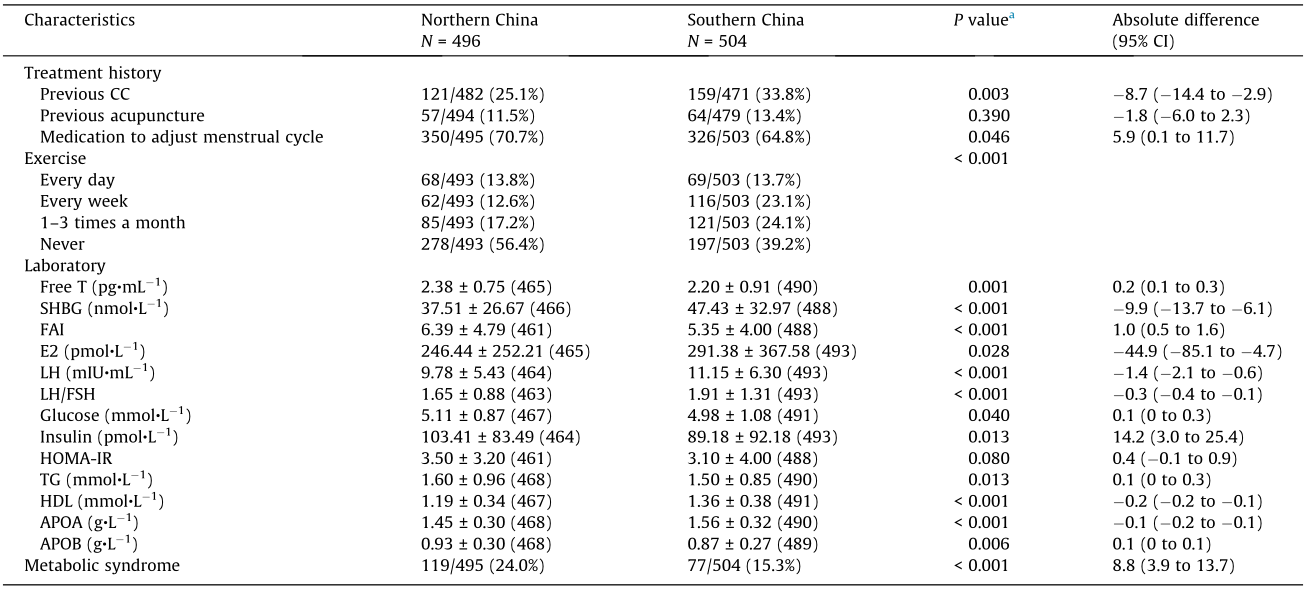
The values in parentheses are total numbers or percentages.
a The Kruskal–Wallis test was used to compare the differences between two groups.
《Table 5》
Table 5 Clinical outcomes by geographic distribution.

a Live birth was defined as the delivery of a live-born infant ≥ 20 weeks’ gestation. Conception was defined as any positive serum level of human chorionic gonadotropin. Pregnancy was defined as an intrauterine pregnancy with fetal heart motion as determined by ultrasonography. Ovulation was defined as a serum progesterone level according to the standard of the local site laboratory (minimum value of luteal phase). Biochemical factor was defined as a positive urine or serum human chorionic gonadotropin test, but no fetus or gestational sac was visible on ultrasound.
b The chi-square test was used to compare the differences between three groups.
《4. Discussion》
4. Discussion
This clinical trial was conducted at 21 sites throughout China and was representative of the entire population of Chinese women with PCOS. This was the largest ever randomized cohort of Chinese PCOS patients. Of the women, 529 had a normal BMI of less than 24, 293 were overweight with a BMI between 24 and 28, and 176 were obese with a BMI greater than 28. There is little genetic, racial, or ethnic variability among Chinese women, but there are significant climate differences between Northern and Southern China that result in different environments and lifestyles between the two populations. There were similar numbers of participants from Northern and Southern China in this trial (496 vs 504 women, respectively).
《4.1. Increased BMI aggravated PCOS phenotypes》
4.1. Increased BMI aggravated PCOS phenotypes
In comparison with a previous study in China that was conducted three years earlier on 644 women with PCOS [16], the participants of the two studies had similar age, BMI, WHR, total T levels, and glucose and lipid profiles. We also compared the difference between the PCOSAct and another previous communitybased epidemiological study in China. We found that subjects of the PCOSAct presented with more severe phenotypes, including higher BMI, higher HOMA-IR, higher hirsutism score, and a higher rate of PCOM. This finding suggests that women with PCOS in a hospital setting present with a more severe phenotype than those in a community setting. Another PCOS cohort in Taiwan Province of China had a similar presentation of PCOS compared with the PCOSAct sample, including similar BMI, WHR, hirsutism score, and reproductive and metabolic hormone levels [17]. A cohort in the Republic of Korea [18] also showed similar BMI and similar prevalence of hyperandrogenemia and PCOM. These findings suggest that women in East Asia share similar phenotypes with ethnic Chinese Han women, resulting in consistent PCOS phenotypes in these populations.
Compared with the participants of two large multicenter trials (Pregnancy in Polycystic Ovary Syndrome (PPCOS) I and II) on infertile women with PCOS that were conducted in the United States and included subjects with different ethnicities and races [19,20], patients in China had significantly lower BMI, T, and hirsutism scores and better lipid profiles. The average BMI of Chinese women was obviously lower than that of American women; however, the 17 Asian participants in PPCOS I had similar phenotypes as the Chinese participants in the PCOSAct. Similarly, the baseline characteristics of the PCOSAct women were comparable with those of PPCOS II with BMI < 30 [21]. This finding indicates the essential role that BMI has in the expression of the PCOS phenotype in different populations around the world.
《4.2. Increased BMI related to decreased intervention effects》
4.2. Increased BMI related to decreased intervention effects
Interestingly, the efficacy of clomiphene on live births was comparable in Chinese women in PCOSAct (28% for four treatment cycles) and in American women with BMI < 30 in PPCOS I (36.8% for six treatment cycles), but the efficacy of clomiphene in Chinese women in PCOSAct was significantly higher than that in the total of American women in PPCOS I when BMI was not considered (28% for four treatment cycles vs 22.5% for six treatment cycles). In PCOSAct, the ovulation rate per treatment cycle was 66.0% in Chinese women with PCOS with a mean BMI of 24.2 [11]. In PPCOS I, the ovulation rate per treatment cycle was 61.0% in a group of Caucasian women with a mean BMI of less than 30.0 [20], and the ovulation rate decreased to 49.0% in obese Caucasian women with a mean BMI of 35.1 [19]. Another study in India showed that the ovulation rate was 56.2% in Indian women with PCOS with a mean BMI of 26.5 [22]. Taken together, all of these studies suggest that the ovulation responses in women with PCOS were consistent with clinical phenotypes and were influenced by BMI, but not by ethnicity.
In the PCOSAct trial, BMI was found to be an important factor in clinical outcomes and, with increased BMI, the rates of ovulation, conception, pregnancy, and live birth were decreased. This was consistent with an IVF cohort study of 239 127 fresh IVF cycles in the United States that showed progressive and statistically significant worsening of pregnancy outcomes in groups with increasing BMI [23]. Recently, lifestyle modification to lose weight before infertility treatment has shown benefits for women with PCOS [24]. Therefore, weight loss should be recommended for PCOS women with a higher BMI who desire to have children.
However, there was no obvious difference between different BMI groups in terms of pregnancy loss rate in the PCOSAct trial, which was similar to another study in China [25]. Nevertheless, a previous study showed that the miscarriage rate was strongly influenced by BMI [26], and obesity has been shown to be an independent factor associated with adverse pregnancy outcomes, including spontaneous miscarriage [27]. Comparing the normal BMI group and the overweight group in the PCOSAct trial, the pregnancy loss rate in the first trimester and the total pregnancy loss rate were significantly increased in the overweight group, but there were no differences between the overweight group and the obese group or between the normal BMI group and the obese group. This might indicate an increased miscarriage risk specifically in overweight women with PCOS.
《4.3. Different lifestyles resulted in different BMI and phenotypes》
4.3. Different lifestyles resulted in different BMI and phenotypes
The significant difference in climate in Northern and Southern China might contribute to the different PCOS phenotypes seen in Chinese women. Overall, women in Northern China had more severe phenotypes and worse treatment outcomes than women in Southern China. We found that the mean body size in Northern China is larger, which can be explained in part by dietary patterns and lifestyle. The northern dietary pattern is characterized by high intakes of wheat, meat, and poultry as staple foods due to the colder climate, and lower intakes of rice, fish, green vegetables, and fresh fruit, compared with the southern dietary pattern that is characterized by high intakes of rice and low intakes of wheat as staple foods [28,29]. Northern Chinese women also engaged in less exercise, likely due to the colder climate, and this was associated with an elevated risk of general and central obesity. Our results showed that increased BMI was strongly associated with the exacerbation of PCOS phenotypes, including more severe insulin resistance, hypertension, dyslipidemia, and varying components of metabolic syndrome. The differences in phenotypes in Northern and Southern Chinese women with PCOS were consistent with the BMI categorizations, so the differences between Northern and Southern China might be explained by the BMI disparity, while some deviations might be explained by cultural factors.
One limitation of this paper is that it was a secondary analysis and was not primarily designed as an epidemiological survey. Another limitation is population mobility, as patients who were enrolled at a local site might not have been born locally. In addition, due to the different acceptance of Chinese medicine, the cohort of PCOS patients might not be homogenous in the northern and southern sites.
This article presents data from the largest hospital-based cohort of women with PCOS and describes the typical phenotypic features and geographic characteristics of women with PCOS from across China. Obesity exacerbated reproductive and metabolic parameters and reduced fecundity among women with PCOS. Different geographic phenotypic features can be explained mostly by differences in BMI and the relationship between BMI and different clinical outcomes.
《Acknowledgements》
Acknowledgements
This study was supported by National Public Welfare Projects for Chinese Medicine (201507001-02), the Heilongjiang Province General Institutes of Higher Education Youth Innovative Talents Program (UNPYSCT-2017226), the Scientific Research Project of Outstanding Innovative Talents Program of Heilongjiang University of Chinese Medicine (2018RC012), Xuzhou Clinical Medical Team Talent Introduction Project—Academician Liu Yixun Integrated Chinese and Western medicine, Maternity and Reproductive Technology Innovation Team, and Academician Liu Yixun Workstation Project.
《Compliance with ethics guidelines》
Compliance with ethics guidelines
Jingshu Gao, Hongli Ma, Yu Wang, Xinming Yang, Yijuan Cao, Bei Zhang, Conghui Han, and Xiaoke Wu declare that they have no conflict of interest or financial conflicts to disclose.














 京公网安备 11010502051620号
京公网安备 11010502051620号