References
[ 1 ]
Konda M, Dodda B, Konala VM, Naramala S, Adapa S. Potential zoonotic origins of SARS-CoV-2 and insights for preventing future pandemics through one health approach. Cureus 2020;12(6):e8932.
link1
[ 2 ]
Lam TTY, Jia N, Zhang YW, Shum MHH, Jiang JF, Zhu HC, et al. Identifying SARS-CoV-2-related coronaviruses in Malayan pangolins. Nature 2020;583 (7815):282–5.
link1
[ 3 ]
Yang Y, Peng F, Wang R, Guan K, Jiang T, Xu G, et al. The deadly coronaviruses: the 2003 SARS pandemic and the 2020 novel coronavirus epidemic in China. J Autoimmun 2020;109:102434.
link1
[ 4 ]
Biziagos E, Passagot J, Crance JM, Deloince R. Long-term survival of hepatitis A virus and poliovirus type 1 in mineral water. Appl Environ Microbiol 1988;54 (11):2705–10.
link1
[ 5 ]
Kauppinen A, Pitkänen T, Miettinen IT. Persistent norovirus contamination of groundwater supplies in two waterborne outbreaks. Food Environ Virol 2018;10(1):39–50.
link1
[ 6 ]
Bøtner A, Belsham GJ. Virus survival in slurry: analysis of the stability of footand-mouth disease, classical swine fever, bovine viral diarrhoea and swine influenza viruses. Vet Microbiol 2012;157(1–2):41–9.
link1
[ 7 ]
Leroy EM, Kumulungui B, Pourrut X, Rouquet P, Hassanin A, Yaba P, et al. Fruit bats as reservoirs of Ebola virus. Nature 2005;438(7068):575–6.
link1
[ 8 ]
Christenson JC, Fischer PR. Beware of bat caves! Marburg hemorrhagic fever in a traveler. Travel Med Advisor 2010;20(4):21–3.
link1
[ 9 ]
Amman BR, Carroll SA, Reed ZD, Sealy TK, Balinandi S, Swanepoel R, et al. Seasonal pulses of Marburg virus circulation in juvenile Rousettus aegyptiacus bats coincide with periods of increased risk of human infection. PLoS Pathog 2012;8(10):e1002877.
link1
[10]
Flyak AI. The analysis of the human antibody response to filovirus infection [dissertation]. Nashville: Vanderbilt University; 2016.
link1
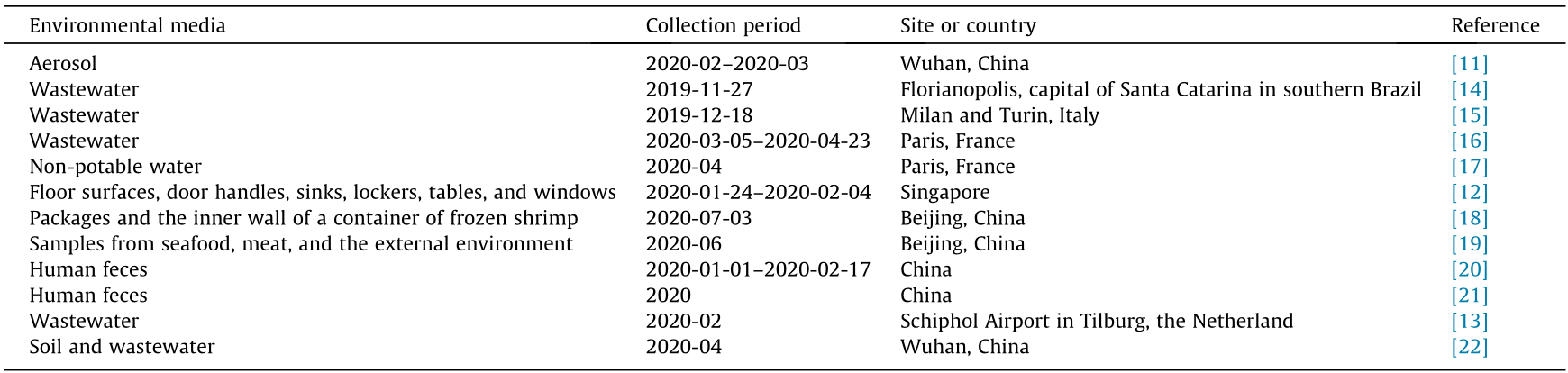
[11]
Liu Y, Ning Z, Chen Y, Guo M, Liu Y, Gali NK, et al. Aerodynamic analysis of SARS-CoV-2 in two Wuhan hospitals. Nature 2020;582(7813):557–60.
link1
[12]
Ong SWX, Tan YK, Chia PY, Lee TH, Ng OT, Wong MSY, et al. Air, surface environmental, and personal protective equipment contamination by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) from a symptomatic patient. JAMA 2020;323(16):1610.
link1
[13]
Mallapaty S. How sewage could reveal true scale of coronavirus outbreak. Nature 2020;580(7802):176–7.
link1
[14]
Fongaro G, Hermes Stoco P, Sobral Marques Souza D, Grisard EC, Magri ME, Rogovski P, et al. SARS-CoV-2 in human sewage in Santa Catalina, Brazil, November 2019. 2020. medRxiv 2020.06.26.2014731.
[15]
Iaconelli M, Bonanno Ferraro G, Mancini P, Veneri C. CS N39/2020 - Studio ISS su acque di scarico, a Milano e Torino Sars-Cov-2 presente già a dicembre [Internet]. Rome: Istituto Superiore di Sanità; 2020 Jun 18 [Cited 2020 Jul 15]. Available from: https://www.iss.it/web/guest/primo-piano/-/asset_publisher/ o4oGR9qmvUz9/content/id/5422725. Italian.
[16]
Wurtzer S, Marechal V, Mouchel J-M, Maday Y, Teyssou R, Richard E, et al. Evaluation of lockdown impact on SARS-CoV-2 dynamics through viral genome quantification in Paris wastewaters. 2020. medRxiv 2020.04.12.20062679.
[17]
Agence France-Presse (AFP). Paris finds ‘minuscule traces’ of coronavirus in its non-potable water [Internet]. Dubai: Al Arabiya Network; 2020 Apr 20 [cited 2020 Jul 15]. Available from: https://english.alarabiya.net/ en/coronavirus/2020/04/20/Paris-finds-minuscule-traces-of-coronavirus-inits-non-potable-water.html.
link1
[18]
CGTN. Coronavirus found on shrimp packaging from Ecuador, China suspends imports from 23 meat companies [Internet]. Beijing: China Global Television Network (CGTN); 2020 Jul 10 [cited 2020 Jul 15]. Available from: https://news.cgtn.com/news/2020-07-10/Coronavirus-found-on-packages-ofshrimps-imported-from-Ecuador-S0O7fXvw4M/index.html.
link1
[19]
Cui H. Coronavirus pandemic: 6 new Beijing cases traced to food market [Internet]. Beijing: China Global Television Network (CGTN); 2020 Jun 13 [cited 2020 Jul 15]. Available from: https://news.cgtn.com/news/ 7855444f7a514464776c6d636a4e6e62684a4856/index.html.
link1
[20]
Wang W, Xu Y, Gao R, Lu R, Han K, Wu G, et al. Detection of SARS-CoV-2 in different types of clinical specimens. JAMA 2020;323(18):1843–4.
link1
[21]
Pan Y, Zhang D, Yang P, Poon LLM, Wang Q. Viral load of SARS-CoV-2 in clinical samples. Lancet Infect Dis 2020;20(4):411–2.
link1
[22]
Zhang D, Yang Y, Huang X, Jiang J, Li M, Zhang X, et al. SARS-CoV-2 spillover into hospital outdoor environments. 2020. medRxiv 2020.05.12.20097105.
[23]
Legendre M, Lartigue A, Bertaux L, Jeudy S, Bartoli J, Lescot M, et al. In-depth study of Mollivirus sibericum, a new 30,000-y-old giant virus infecting Acanthamoeba. Proc Natl Acad Sci USA 2015;112(38):E5327–35.
link1
[24]
Hurst CJ, Gerba CP, Cech I. Effects of environmental variables and soil characteristics on virus survival in soil. Appl Environ Microbiol 1980;40 (6):1067–79.
link1
[25]
Seitz SR, Leon JS, Schwab KJ, Lyon GM, Dowd M, McDaniels M, et al. Norovirus infectivity in humans and persistence in water. Appl Environ Microbiol 2011;77(19):6884–8.
link1
[26]
McDaniels AE, Cochran KW, Gannon JJ, Williams GW. Rotavirus and reovirus stability in microorganism-free distilled and waste waters. Water Res 1983;17(10):1349–53.
link1
[27]
Abad FX, Pintó RM, Villena C, Gajardo R, Bosch A. Astrovirus survival in drinking water. Appl Environ Microbiol 1997;63(8):3119–22.
link1
[28]
Zarkov IS. Survival of avian influenza viruses in filtered and natural surface waters of different physical and chemical parameters. Rev Med Vet 2006;157 (10):471–6.
link1
[29]
Akers TG, Prato CM, Dubovi EJ. Airborne stability of simian virus 40. Appl Microbiol 1973;26(2):146–8.
link1
[30]
Ahne W. Comparative studies of the stability of 4 fish-pathogenic viruses (VHSV, PFR, SVCV, IPNV). Zentralbl Veterinarmed B 1982;29(6):457–76. German.
[31]
Wu S, Yan Y, Yan P, Den Y, Chen L. Study on the survival ability of HIV in the micro environment of biological safety laboratory. Chin J Exp Clin Virol 2014;28(6):426–8.
link1
[32]
Curry SS, Brown DR, Gaskin JM, Jacobson ER, Ehrhart LM, Blahak S, et al. Persistent infectivity of a disease-associated herpesvirus in green turtles after exposure to seawater. J Wildl Dis 2000;36(4):792–7.
link1
[33]
Hawley LM, Garver KA. Stability of viral hemorrhagic septicemia virus (VHSV) in freshwater and seawater at various temperatures. Dis Aquat Organ 2008;82(3):171–8.
link1
[34]
Dayaram A, Franz M, Schattschneider A, Damiani AM, Bischofberger S, Osterrieder N, et al. Long term stability and infectivity of herpesviruses in water. Sci Rep 2017;7(1):46559.
link1
[35]
Firquet S, Beaujard S, Lobert PE, Sané F, Caloone D, Izard D, et al. Survival of enveloped and non-enveloped viruses on inanimate surfaces. Microbes Environ 2015;30(2):140–4.
link1
[36]
Chung H, Sobsey MD. Comparative survival of indicator viruses and enteric viruses in seawater and sediment. Water Sci Technol 1993;27(3–4): 425–8.
link1
[37]
Dee SA, Martinez BC, Clanton C. Survival and infectivity of porcine reproductive and respiratory syndrome virus in swine lagoon effluent. Vet Rec 2005;156(2):56–7.
link1
[38]
Francis DP, Essex M, Gayzagian D. Feline leukemia virus: survival under home and laboratory conditions. J Clin Microbiol 1979;9(1):154–6.
link1
[39]
Butot S, Putallaz T, Sánchez G. Effects of sanitation, freezing and frozen storage on enteric viruses in berries and herbs. Int J Food Microbiol 2008;126 (1–2):30–5.
link1
[40]
Ding DC, Chang YC, Liu HW, Chu TY. Long-term persistence of human papillomavirus in environments. Gynecol Oncol 2011;121(1):148–51.
link1
[41]
Hernández A, Marina CF, Valle J, Williams T. Persistence of invertebrate iridescent virus 6 in tropical artificial aquatic environments. Brief report. Arch Virol 2005;150(11):2357–63.
link1
[42]
Hurst CJ, Benton WH, McClellan KA. Thermal and water source effects upon the stability of enteroviruses in surface freshwaters. Can J Microbiol 1989;35 (4):474–80.
link1
[43]
Doerrbecker J, Behrendt P, Mateu-Gelabert P, Ciesek S, Riebesehl N, Wilhelm C, et al. Transmission of hepatitis C virus among people who inject drugs: viral stability and association with drug preparation equipment. J Infect Dis 2013;207(2):281–7.
link1
[44]
Hick P, Evans O, Looi R, English C, Whittington RJ. Stability of Ostreid herpesvirus-1 (OsHV-1) and assessment of disinfection of seawater and oyster tissues using a bioassay. Aquaculture 2016;450:412–21.
link1
[45]
Arthur SE, Gibson KE. Environmental persistence of Tulane virus—a surrogate for human norovirus. Can J Microbiol 2016;62(5):449–54.
link1
[46]
Esseili MA, Saif LJ, Farkas T, Wang Q. Feline calicivirus, murine norovirus, porcine sapovirus, and tulane virus survival on postharvest lettuce. Appl Environ Microbiol 2015;81(15):5085–92.
link1
[47]
Hyslop NSG. Observations on the survival and infectivity of airborne rinderpest virus. Int J Biometeorol 1979;23(1):1–7.
link1
[48]
Broadbent L, Fletcher JT. The epidemiology of tomato mosaic: IV. persistence of virus on clothing and glasshouse structures. Ann Appl Biol 1963;52 (2):233–41.
link1
[49]
Damgaardlarsen S, Jensen KO, Lund E, Nissen B. Survival and movement of enterovirus in connection with land disposal of sludges. Water Res 1977;11 (6):503–8.
link1
[50]
Guan J, Chan M, Brooks BW, Spencer JL. Infectious bursal disease virus as a surrogate for studies on survival of various poultry viruses in compost. Avian Dis 2010;54(2):919–22.
link1
[51]
Ijaz MK, Sattar SA, Alkarmi T, Dar FK, Bhatti AR, Elhag KM. Studies on the survival of aerosolized bovine rotavirus (UK) and a murine rotavirus. Comp Immunol Microbiol Infect Dis 1994;17(2):91–8.
link1
[52]
Brown P, Gajdusek DC. Survival of scrapie virus after 3 years’ interment. Lancet 1991;337(8736):269–70.
link1
[53]
Baert L, Uyttendaele M, Vermeersch M, Van Coillie E, Debevere J. Survival and transfer of murine norovirus 1, a surrogate for human noroviruses, during the production process of deep-frozen onions and spinach. J Food Prot 2008;71 (8):1590–7.
link1
[54]
Ricklin ME, García-Nicolás O, Brechbühl D, Python S, Zumkehr B, Nougairede A, et al. Vector-free transmission and persistence of Japanese encephalitis virus in pigs. Nat Commun 2016;7(1):10832.
link1
[55]
Jordan FT, Nassar TJ. The survival of infectious bronchitis (IB) virus in water. Avian Pathol 1973;2(2):91–101.
link1
[56]
Paek MR, Lee YJ, Yoon H, Kang HM, Kim MC, Choi JG, et al. Survival rate of H5N1 highly pathogenic avian influenza viruses at different temperatures. Poult Sci 2010;89(8):1647–50.
link1
[57]
Bibby K, Casson LW, Stachler E, Haas CN. Ebola virus persistence in the environment: state of the knowledge and research needs. Environ Sci Technol Lett 2015;2(1):2–6.
link1
[58]
Lotlikar MS, Lipson SM. Survival of spumavirus, a primate retrovirus, in laboratory media and water. FEMS Microbiol Lett 2002;211(2):207–11.
link1
[59]
Liang L, Goh SG, Gin KYH. Decay kinetics of microbial source tracking (MST) markers and human adenovirus under the effects of sunlight and salinity. Sci Total Environ 2017;574:165–75.
link1
[60]
Brown JD, Swayne DE, Cooper RJ, Burns RE, Stallknecht DE. Persistence of H5 and H7 avian influenza viruses in water. Avian Dis 2007;51(1 Suppl):285–9.
link1
[61]
Stallknecht DE, Shane SM, Kearney MT, Zwank PJ. Persistence of avian influenza viruses in water. Avian Dis 1990;34(2):406–11.
link1
[62]
Mehle N, Gutiérrez-Aguirre I, Prezelj N, Delic D, Vidic U, Ravnikar M. Survival and transmission of potato virus Y, pepino mosaic virus, and potato spindle tuber viroid in water. Appl Environ Microbiol 2014;80(4):1455–62.
link1
[63]
Parkinson AJ, Muchmore HG, Scott EN, Scott LV. Survival of human parainfluenza viruses in the South Polar environment. Appl Environ Microbiol 1983;46(4):901–5.
link1
[64]
Paluszak Z, Lipowski A, Ligocka A. Survival rate of Suid herpesvirus (SuHV-1, Aujeszky’s disease virus, ADV) in composted sewage sludge. Pol J Vet Sci 2012;15(1):51–4.
link1
[65]
Dublineau A, Batéjat C, Pinon A, Burguière AM, Leclercq I, Manuguerra JC. Persistence of the 2009 pandemic influenza A (H1N1) virus in water and on non-porous surface. PLoS ONE 2011;6(11):e28043.
link1
[66]
Lebarbenchon C, Yang M, Keeler SP, Ramakrishnan MA, Brown JD, Stallknecht DE, et al. Viral replication, persistence in water and genetic characterization of two influenza A viruses isolated from surface lake water. PLoS ONE 2011;6 (10):e26566.
link1
[67]
Sagripanti JL, Rom AM, Holland LE. Persistence in darkness of virulent alphaviruses, Ebola virus, and Lassa virus deposited on solid surfaces. Arch Virol 2010;155(12):2035–9.
link1
[68]
Reagan KJ, McGeady ML, Crowell RL. Persistence of human rhinovirus infectivity under diverse environmental conditions. Appl Environ Microbiol 1981;41(3):618–20.
link1
[69]
Graiver DA, Topliff CL, Kelling CL, Bartelt-Hunt SL. Survival of the avian influenza virus (H6N2) after land disposal. Environ Sci Technol 2009;43 (11):4063–7.
link1
[70]
Stowell JD, Forlin-Passoni D, Radford K, Bate SL, Dollard SC, Bialek SR, et al. Cytomegalovirus survival and transferability and the effectiveness of common hand-washing agents against cytomegalovirus on live human hands. Appl Environ Microbiol 2014;80(2):455–61.
link1
[71]
Shoham D, Jahangir A, Ruenphet S, Takehara K. Persistence of avian influenza viruses in various artificially frozen environmental water types. Influenza Res Treat 2012;2012:912326.
link1
[72]
Zhang H, Li Y, Chen J, Chen Q, Chen Z. Perpetuation of H5N1 and H9N2 avian influenza viruses in natural water bodies. J Gen Virol 2014;95(Pt 7):1430–5.
link1
[73]
Belanov EF, Muntianov VP, Kriuk VD, Sokolov AV, Bormotov NI, P’iankov OV, et al. Survival of Marburg virus infectivity on contaminated surfaces and in aerosols. Vopr Virusol 1996;41(1):32–4. Russian.
[74]
Calnek BW, Hitchner SB. Survival and disinfection of Marek’s disease virus and the effectiveness of filters in preventing airborne dissemination. Poult Sci 1973;52(1):35–43.
link1
[75]
Casanova L, Rutala WA, Weber DJ, Sobsey MD. Survival of surrogate coronaviruses in water. Water Res 2009;43(7):1893–8.
link1
[76]
Oidtmann B, Dixon P, Way K, Joiner C, Bayley AE. Risk of waterborne virus spread—review of survival of relevant fish and crustacean viruses in the aquatic environment and implications for control measures. Rev Aquacult 2018;10(3):641–69.
link1
[77]
van Doremalen N, Bushmaker T, Morris DH, Holbrook MG, Gamble A, Williamson BN, et al. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med 2020;382(16):1564–7.
link1
[78]
Cottral GE. Persistence of foot-and-mouth disease virus in animals, their products and the environment. Bull Off Int Epizoot 1969;71(3–4):549–68.
link1
[79]
Wang XW, Li JS, Jin M, Zhen B, Kong QX, Song N, et al. Study on the resistance of severe acute respiratory syndrome-associated coronavirus. J Virol Methods 2005;126(1–2):171–7.
link1
[80]
De Jong JG, Winkler KC. Survival of measles virus in air. Nature 1964;201 (4923):1054–5.
link1
[81]
St-Hilaire S, Beevers N, Way K, Le Deuff RM, Martin P, Joiner C. Reactivation of koi herpesvirus infections in common carp Cyprinus carpio. Dis Aquat Organ 2005;67(1–2):15–23.
link1
[82]
Zimmer B, Summermatter K, Zimmer G. Stability and inactivation of vesicular stomatitis virus, a prototype rhabdovirus. Vet Microbiol 2013;162(1):78–84.
link1
[83]
van Doremalen N, Bushmaker T, Munster VJ. Stability of Middle East respiratory syndrome coronavirus (MERS-CoV) under different environmental conditions. Euro Surveill 2013;18(38):20590.
link1
[84]
Harcourt DG, Cass LM. Persistence of a granulosis virus of Pieris rapae in soil. J Invertebr Pathol 1968;11(1):142–3.
link1
[85]
Escudero BI, Rawsthorne H, Gensel C, Jaykus LA. Persistence and transferability of noroviruses on and between common surfaces and foods. J Food Prot 2012;75(5):927–35.
link1
[86]
Smither SJ, Eastaugh LS, Findlay JS, O’Brien LM, Thom R, Lever MS. Survival and persistence of Nipah virus in blood and tissue culture media. Emerg Microbes Infect 2019;8(1):1760–2.
link1
[87]
Davis-Fields MK, Allison AB, Brown JR, Poulson RL, Stallknecht DE. Effects of temperature and pH on the persistence of avian paramyxovirus-1 in water. J Wildl Dis 2014;50(4):998–1000.
link1
[88]
Kallio ER, Klingström J, Gustafsson E, Manni T, Vaheri A, Henttonen H, et al. Prolonged survival of Puumala hantavirus outside the host: evidence for indirect transmission via the environment. J Gen Virol 2006;87(Pt 8):2127–34.
link1
[89]
Demangeat G, Voisin R, Minot JC, Bosselut N, Fuchs M, Esmenjaud D. Survival of Xiphinema index in vineyard soil and retention of Grapevine fanleaf virus over extended time in the absence of host plants. Phytopathology 2005;95 (10):1151–6.
link1
[90]
Friedrich R, Kaemmerer D, Seigner L. Investigation of the persistence of Beet necrotic yellow vein virus in rootlets of sugar beet during biogas fermentation. J Plant Dis Prot 2010;117(4):150–5.
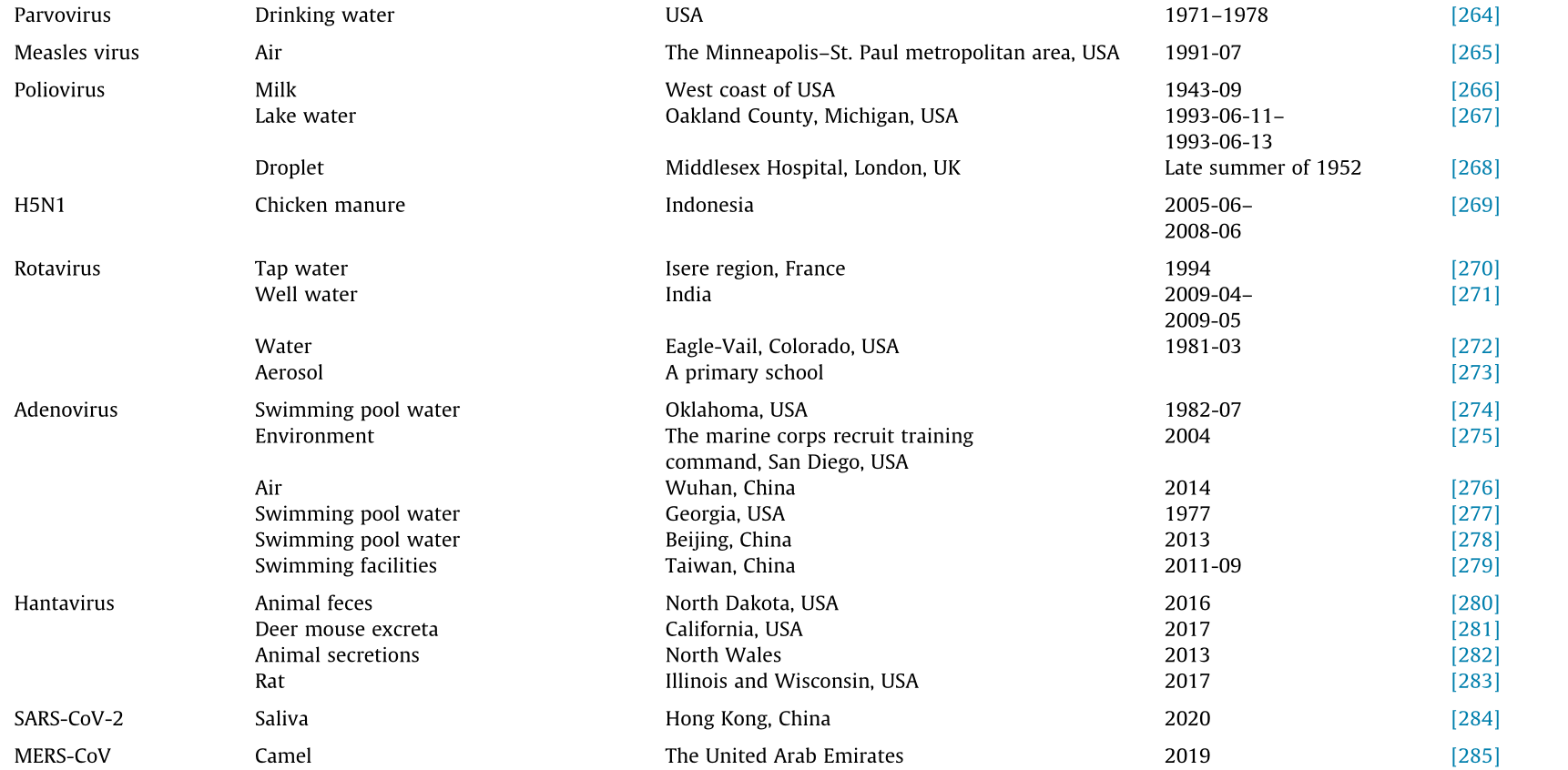
link1
[91]
Zhang Q, Li J, Jiang X, Li C, Liu L, Liang M, et al. A primary study of the thermal stability and inactivation of severe fever with thrombocytopenia syndrome virus. Chin J Exp Clin Virol 2014;28(3):206–8.
link1
[92]
Bitterlin MW, Gonsalves D. Spatial distribution of Xiphinema rivesi and persistence of tomato ringspot virus and its vector in soil. Plant Dis 1987;71 (5):408–11.
link1
[93]
Graham DA, Staples C, Wilson CJ, Jewhurst H, Cherry K, Gordon A, et al. Biophysical properties of salmonid alphaviruses: influence of temperature and pH on virus survival. J Fish Dis 2007;30(9):533–43.
link1
[94]
Thomas Y, Vogel G, Wunderli W, Suter P, Witschi M, Koch D, et al. Survival of influenza virus on banknotes. Appl Environ Microbiol 2008;74(10):3002–7.
link1
[95]
Gundy PM, Gerba CP, Pepper IL. Survival of coronaviruses in water and wastewater. Food Environ Virol 2009;1(1):10–4.
link1
[96]
Thompson CG, Scott DW, Wickman BE. Long-term persistence of the nuclear polyhedrosis virus of the Douglas-fir tussock moth, Orgyia pseudotsugata (Lepidoptera: Lymantriidae), in forest soil. Environ Entomol 1981;10 (2):254–5.
link1
[97]
Huq F. Effect of temperature and relative humidity on variola virus in crusts. Bull World Health Organ 1976;54(6):710–2.
link1
[98]
Karalyan Z, Avetisyan A, Avagyan H, Ghazaryan H, Vardanyan T, Manukyan A, et al. Presence and survival of African swine fever virus in leeches. Vet Microbiol 2019;237:108421.
link1
[99]
Espinosa AC, Mazari-Hiriart M, Espinosa R, Maruri-Avidal L, Méndez E, Arias CF. Infectivity and genome persistence of rotavirus and astrovirus in groundwater and surface water. Water Res 2008;42(10–11):2618–28.
link1
[100]
Mebus CA, House C, Gonzalvo FR, Pineda JM, Tapiador J, Pire JJ, et al. Survival of swine vesicular disease virus in Spanish Serrano cured hams and Iberian cured hams, shoulders and loins. Food Microbiol 1993;10(3):263–8.
link1
[101]
Munro J, Bayley AE, McPherson NJ, Feist SW. Survival of frog virus 3 in freshwater and sediment from an English lake. J Wildl Dis 2016;52 (1):138–42.
link1
[102]
Momoyama K. Survival of baculoviral mid-gut gland necrosis virus (BMNV) in infected tissues and in sea water. Fish Pathol 1989;24(3):179–81.
link1
[103]
Jones TH, Muehlhauser V. Survival of Porcine teschovirus as a surrogate virus on pork chops during storage at 2 C. Int J Food Microbiol 2015;194:21–4.
link1
[104]
Ogaard L, Williams CF, Payne CC, Zethner O. Activity persistence of granulosis viruses [Baculoviridae] in soils in United Kingdom and Denmark. Entomophaga 1988;33(1):73–80.
link1
[105]
Kumar SS, Bharathi RA, Rajan JJS, Alavandi SV, Poornima M, Balasubramanian CP, et al. Viability of white spot syndrome virus (WSSV) in sediment during sun-drying (drainable pond) and under non-drainable pond conditions indicated by infectivity to shrimp. Aquaculture 2013;402:119–26.
link1
[106]
Pietsch JP, Amend DF, Miller CM. Survival of infectious hematopoietic necrosis virus held under various environmental conditions. J Fish Res Board Can 1977;34(9):1360–4.
link1
[107]
Leiva-Rebollo R, Labella AM, Valverde EJ, Castro D, Borrego JJ. Persistence of lymphocystis disease virus (LCDV) in seawater. Food Environ Virol 2020;12 (2):174–9.
link1
[108]
Long PH, Olitsky PK. Effect of cysteine on the survival of vaccine virus. Proc Soc Exp Biol Med 1930;27(5):380–1.
link1
[109]
Miles SL, Takizawa K, Gerba CP, Pepper IL. Survival of infectious prions in water. J Environ Sci Health A Tox Hazard Subst Environ Eng 2011;46(9):938–43.
link1
[110]
Mor SK, Verma H, Sharafeldin TA, Porter RE, Ziegler AF, Noll SL, et al. Survival of turkey arthritis reovirus in poultry litter and drinking water. Poult Sci 2015;94(4):639–42.
link1
[111]
Nath Srivastava R, Lund E. The stability of bovine parvovirus and its possible use as an indicator for the persistence of enteric viruses. Water Res 1980;14 (8):1017–21.
link1
[112]
Olszewska H, Paluszak Z, Jarzabek Z. Survival of bovine enterovirus strain LCR-4 in water, slurry, and soil. Bull Vet Inst Pulawy 2008;52(2):205–9.
link1
[113]
Parashar D, Khalkar P, Arankalle VA. Survival of hepatitis A and E viruses in soil samples. Clin Microbiol Infect 2011;17(11):E1–4.
link1
[114]
Plumb JA, Wright LD, Jones VL. Survival of channel catfish virus in chilled, frozen, and decomposing channel catfish. Prog Fish Cult 1973;35(3):170–2.
link1
[115]
Savage CE, Jones RC. The survival of avian reoviruses on materials associated with the poultry house environment. Avian Pathol 2003;32(4):419–25.
link1
[116]
Tapia E, Monti G, Rozas M, Sandoval A, Gaete A, Bohle H, et al. Assessment of the in vitro survival of the infectious salmon anaemia virus (ISAV) under different water types and temperature. Bull Eur Assoc Fish Pathol 2013;33 (1):3–12.
link1
[117]
Tu KC, Spendlove RS, Goede RW. Effect of temperature on survival and growth of infectious pancreatic necrosis virus. Infect Immun 1975;11 (6):1409–12.
link1
[118]
Uttenthal A, Lund E, Hansen M. Mink enteritis parvovirus. Stability of virus kept under outdoor conditions. APMIS 1999;107(3):353–8.
link1
[119]
Wolf K, Burke CN. Survival of duck plague virus in water from Lake Andes National Wildlife Refuge, South Dakota. J Wildl Dis 1982;18(4):437–40.
link1
[120]
Mather T, Takeda T, Tassello J, Ohagen A, Serebryanik D, Kramer E, et al. West Nile virus in blood: stability, distribution, and susceptibility to PEN110 inactivation. Transfusion 2003;43(8):1029–37.
link1
[121]
Liu H, Xiong C, Chen J, Chen G, Zhang J, Li Y, et al. Two genetically diverse H7N7 avian influenza viruses isolated from migratory birds in central China. Emerg Microbes Infect 2018;7(1):62.
link1
[122]
Than TT, Jo E, Todt D, Nguyen PH, Steinmann J, Steinmann E, et al. High environmental stability of hepatitis B virus and inactivation requirements for chemical biocides. J Infect Dis 2019;219(7):1044–8.
link1
[123]
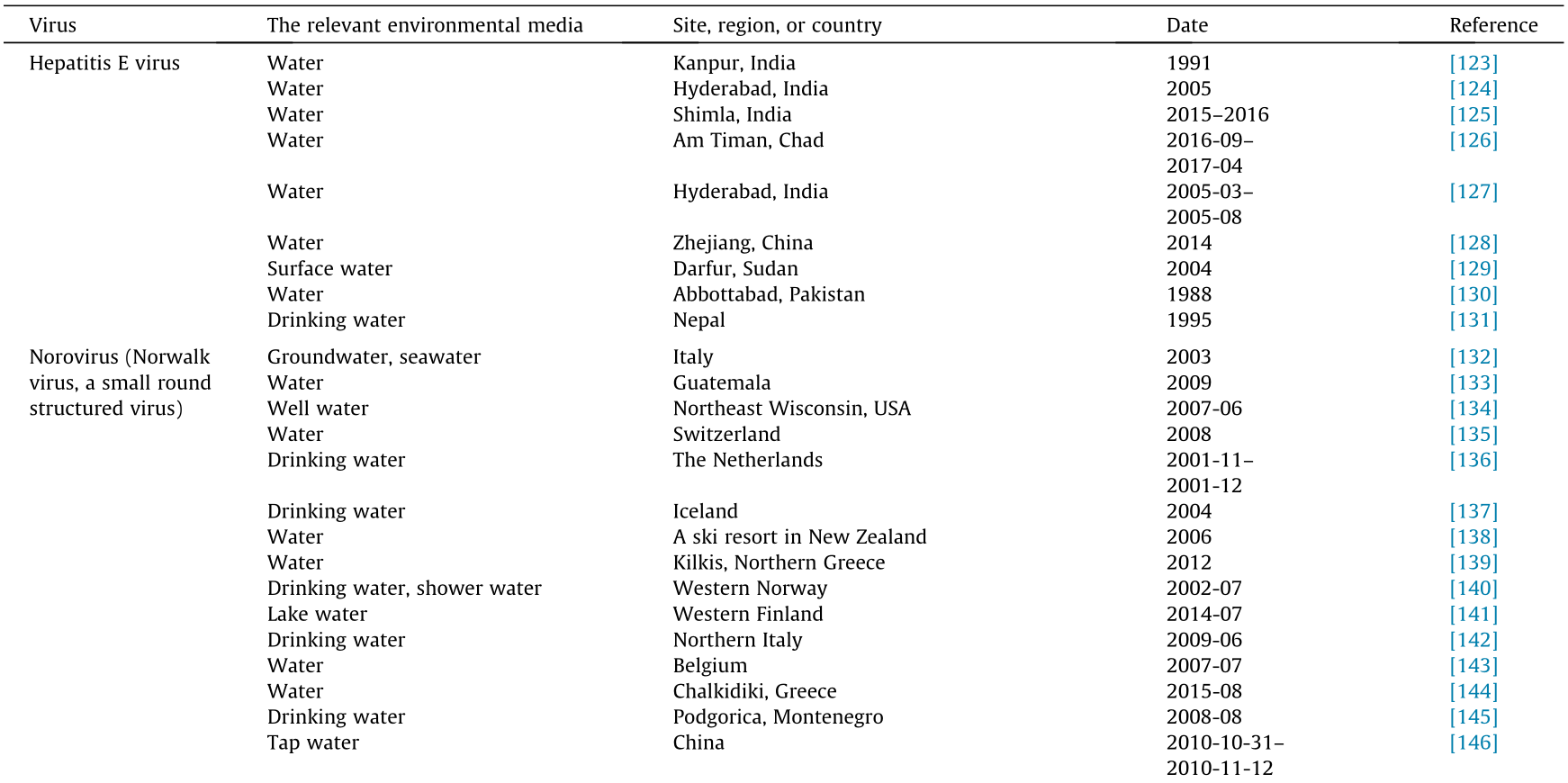
Aggarwal R, Naik SR. Hepatitis E: intrafamilial transmission versus waterborne spread. J Hepatol 1994;21(5):718–23.
link1
[124]
Sailaja B, Murhekar MV, Hutin YJ, Kuruva S, Murthy SP, Reddy KSJ, et al. Outbreak of waterborne hepatitis E in Hyderabad, India, 2005. Epidemiol Infect 2009;137(2):234–40.
link1
[125]
Tripathy AS, Sharma M, Deoshatwar AR, Babar P, Bharadwaj R, Bharti OK. Study of a hepatitis E virus outbreak involving drinking water and sewage contamination in Shimla, India, 2015–2016. Trans R Soc Trop Med Hyg 2019;113(12):789–96.
link1
[126]
Lenglet A, Ehlkes L, Taylor D, Fesselet JF, Nassariman JN, Ahamat A, et al. Does community-wide water chlorination reduce hepatitis E virus infections during an outbreak? A geospatial analysis of data from an outbreak in Am Timan, Chad (2016–2017). J Water Health 2020;18(4):556–65.
link1
[127]
Sarguna P, Rao A, Sudha Ramana KN. Outbreak of acute viral hepatitis due to hepatitis E virus in Hyderabad. Indian J Med Microbiol 2007;25(4):378–82.
link1
[128]
Chen YJ, Cao NX, Xie RH, Ding CX, Chen EF, Zhu HP, et al. Epidemiological investigation of a tap water-mediated hepatitis E virus genotype 4 outbreak in Zhejiang Province, China. Epidemiol Infect 2016;144(16):3387–99.
link1
[129]
Guthmann JP, Klovstad H, Boccia D, Hamid N, Pinoges L, Nizou JY, et al. A large outbreak of hepatitis E among a displaced population in Darfur, Sudan, 2004: the role of water treatment methods. Clin Infect Dis 2006;42 (12):1685–91.
link1
[130]
Bryan JP, Iqbal M, Tsarev S, Malik IA, Duncan JF, Ahmed A, et al. Epidemic of hepatitis E in a military unit in Abbotrabad, Pakistan. Am J Trop Med Hyg 2002;67(6):662–8.
link1
[131]
Clayson ET, Vaughn DW, Innis BL, Shrestha MP, Pandey R, Malla DB. Association of hepatitis E virus with an outbreak of hepatitis at a military training camp in Nepal. J Med Virol 1998;54(3):178–82.
link1
[132]
Migliorati G, Prencipe V, Ripani A, Di Francesco C, Casaccia C, Crudeli S, et al. An outbreak of gastroenteritis in a holiday resort in Italy: epidemiological survey, implementation and application of preventive measures. Vet Ital 2008;44(3):469–81.
link1
[133]
Arvelo W, Sosa SM, Juliao P, López MR, Estevéz A, López B, et al. Norovirus outbreak of probable waterborne transmission with high attack rate in a Guatemalan resort. J Clin Virol 2012;55(1):8–11.
link1
[134]
Borchardt MA, Bradbury KR, Alexander EC Jr, Kolberg RJ, Alexander SC, Archer JR, et al. Norovirus outbreak caused by a new septic system in a dolomite aquifer. Ground Water 2011;49(1):85–97.
link1
[135]
Breitenmoser A, Fretz R, Schmid J, Besl A, Etter R. Outbreak of acute gastroenteritis due to a washwater-contaminated water supply, Switzerland, 2008. J Water Health 2011;9(3):569–76.
link1
[136]
Fernandes TMA, Schout C, De Roda Husman AM, Eilander A, Vennema H, van Duynhoven YTHP. Gastroenteritis associated with accidental contamination of drinking water with partially treated water. Epidemiol Infect 2007;135 (5):818–26.
link1
[137]
Gunnarsdottir MJ, Gardarsson SM, Andradottir HO. Microbial contamination in groundwater supply in a cold climate and coarse soil: case study of norovirus outbreak at Lake Myvatn, Iceland. Hydrol Res 2013;44(6):1114–28.
link1
[138]
Hewitt J, Bell D, Simmons GC, Rivera-Aban M, Wolf S, Greening GE. Gastroenteritis outbreak caused by waterborne norovirus at a New Zealand ski resort. Appl Environ Microbiol 2007;73(24):7853–7.
link1
[139]
Mellou K, Sideroglou T, Potamiti-Komi M, Kokkinos P, Ziros P, Georgakopoulou T, et al. Epidemiological investigation of two parallel gastroenteritis outbreaks in school settings. BMC Public Health 2013;13(1):241.
link1
[140]
Nygård K, Vold L, Halvorsen E, Bringeland E, Røttingen JA, Aavitsland P. Waterborne outbreak of gastroenteritis in a religious summer camp in Norway, 2002. Epidemiol Infect 2004;132(2):223–9.
link1
[141]
Polkowska A, Räsänen S, Al-Hello H, Bojang M, Lyytikäinen O, Nuorti JP, et al. An outbreak of norovirus infections associated with recreational lake water in Western Finland, 2014. Epidemiol Infect 2018;146(5):544–50.
link1
[142]
Scarcella C, Carasi S, Cadoria F, Macchi L, Pavan A, Salamana M, et al. An outbreak of viral gastroenteritis linked to municipal water supply, Lombardy, Italy, June 2009. Euro Surveill 2009;14(29):15–7.
link1
[143]
ter Waarbeek HLG, Dukers-Muijrers NHTM, Vennema H, Hoebe CJPA. Waterborne gastroenteritis outbreak at a scouting camp caused by two norovirus genogroups: GI and GII. J Clin Virol 2010;47(3):268–72.
link1
[144]
Tryfinopoulou K, Kyritsi M, Mellou K, Kolokythopoulou F, Mouchtouri VA, Potamiti-Komi M, et al. Norovirus waterborne outbreak in Chalkidiki, Greece, 2015: detection of GI.P2_GI.2 and GII.P16_GII.13 unusual strains. Epidemiol Infect 2019;147:e227.
[145]
Werber D, Lausevic´ D, Mugosa B, Vratnica Z, Ivanovic´ -Nikolic´ L, Zizic´ L, et al. Massive outbreak of viral gastroenteritis associated with consumption of municipal drinking water in a European capital city. Epidemiol Infect 2009;137(12):1713–20.
link1
[146]
Yang Z, Wu X, Li T, Li M, Zhong Y, Liu Y, et al. Epidemiological survey and analysis on an outbreak of gastroenteritis due to water contamination. Biomed Environ Sci 2011;24(3):275–83.
link1
[147]
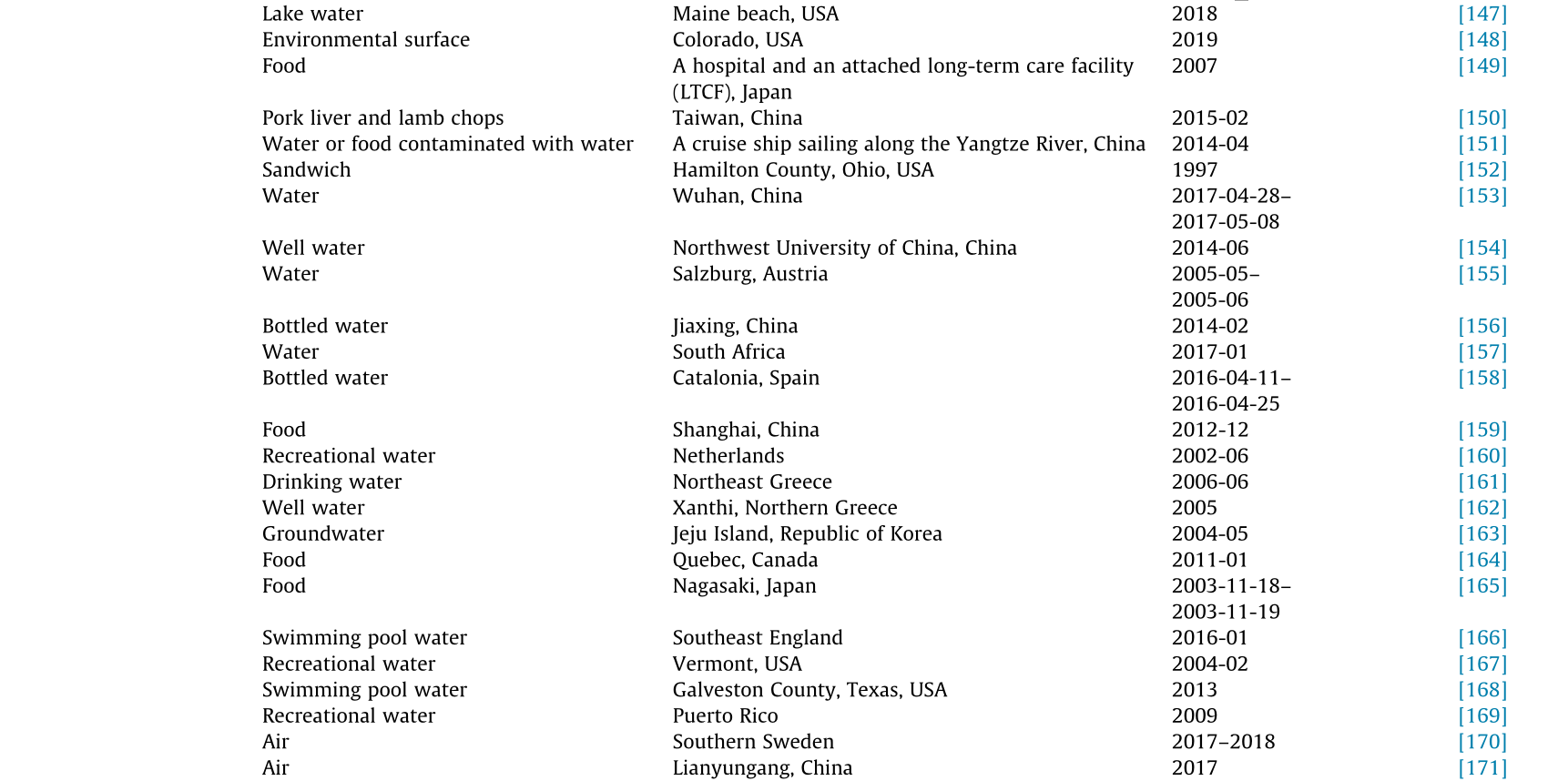
Centers for Disease Control (CDC). Outbreaks associated with untreated recreational water—California, Maine, and Minnesota, 2018–2019. MMWR Morb Mortal Wkly Rep 2020;69(25):781–3.
[148]
Pawlowski A. Suspected norovirus outbreak shuts down Colorado school district [Internet]. New York: NBC News; 2019 Nov 21 [cited 2020 Jul 15]. Available from: https://www.newsbreak.com/news/1462358518070/ suspected norovirus-outbreak-shuts-down-colorado-school-district.
link1
[149]
Ohwaki K, Nagashima H, Aoki M, Aoki H, Yano E. A foodborne norovirus outbreak at a hospital and an attached long-term care facility. Jpn J Infect Dis 2009;62(6):450.
link1
[150]
Chen MY, Chen WC, Chen PC, Hsu SW, Lo YC. An outbreak of norovirus gastroenteritis associated with asymptomatic food handlers in Kinmen, Taiwan. BMC Public Health 2016;16(1):372.
link1
[151]
Wang X, Yong W, Shi L, Qiao M, He M, Zhang H, et al. An outbreak of multiple norovirus strains on a cruise ship in China, 2014. J Appl Microbiol 2016;120 (1):226–33.
link1
[152]
Parashar UD, Dow L, Fankhauser RL, Humphrey CD, Miller J, Ando T, et al. An outbreak of viral gastroenteritis associated with consumption of sandwiches: implications for the control of transmission by food handlers. Epidemiol Infect 1998;121(3):615–21.
link1
[153]
Zhou X, Kong DG, Li J, Pang BB, Zhao Y, Zhou JB, et al. An outbreak of gastroenteritis associated with GII.17 norovirus-contaminated secondary water supply system in Wuhan, China, 2017. Food Environ Virol 2019;11 (2):126–37.
[154]
Zhang L, Li X, Wu R, Chen H, Liu J, Wang Z, et al. A gastroenteritis outbreak associated with drinking water in a college in northwest China. J Water Health 2018;16(4):508–15.
link1
[155]
Schmid D, Lederer I, Much P, Pichler AM, Allerberger F. Outbreak of norovirus infection associated with contaminated flood water, Salzburg, 2005. Euro Surveill 2005;10(6): E050616.3.
link1
[156]
Shang X, Fu X, Zhang P, Sheng M, Song J, He F, et al. An outbreak of norovirus-associated acute gastroenteritis associated with contaminated barrelled water in many schools in Zhejiang, China. PLoS ONE 2017;12(2): e0171307.
link1
[157]
Sekwadi PG, Ravhuhali KG, Mosam A, Essel V, Ntshoe GM, Shonhiwa AM, et al. Waterborne outbreak of gastroenteritis on the KwaZulu–Natal Coast, South Africa, December 2016/January 2017. Epidemiol Infect 2018;146 (10):1318–25.
link1
[158]
Blanco A, Guix S, Fuster N, Fuentes C, Bartolomé R, Cornejo T, et al. Norovirus in bottled water associated with gastroenteritis outbreak, Spain, 2016. Emerg Infect Dis 2017;23(9):1531–4.
link1
[159]
Xue C, Fu Y, Zhu W, Fei Y, Zhu L, Zhang H, et al. An outbreak of acute norovirus gastroenteritis in a boarding school in Shanghai: a retrospective cohort study. BMC Public Health 2014;14(1):1092.
link1
[160]
Hoebe CJPA, Vennema H, de Roda Husman AM, van Duynhoven YTHP. Norovirus outbreak among primary schoolchildren who had played in a recreational water fountain. J Infect Dis 2004;189(4):699–705.
link1
[161]
Vantarakis A, Mellou K, Spala G, Kokkinos P, Alamanos Y. A gastroenteritis outbreak caused by noroviruses in Greece. Int J Environ Res Public Health 2011;8(8):3468–78.
link1
[162]
Papadopoulos VP, Vlachos O, Isidoriou E, Kasmeridis C, Pappa Z, Goutzouvelidis A, et al. A gastroenteritis outbreak due to norovirus infection in Xanthi, Northern Greece: management and public health consequences. J Gastrointestin Liver Dis 2006;15(1):27–30.
link1
[163]
Kim SH, Cheon DS, Kim JH, Lee DH, Jheong WH, Heo YJ, et al. Outbreaks of gastroenteritis that occurred during school excursions in Korea were associated with several waterborne strains of norovirus. J Clin Microbiol 2005;43(9):4836–9.
link1
[164]
Gaulin C, Nguon S, Leblanc MA, Ramsay D, Roy S. Multiple outbreaks of gastroenteritis that were associated with 16 funerals and a unique caterer and spanned 6 days, 2011, Québec. Canada. J Food Prot 2013;76 (9):1582–9.
link1
[165]
Hirakata Y, Arisawa K, Nishio O, Nakagomi O. Multiprefectural spread of gastroenteritis outbreaks attributable to a single genogroup II norovirus strain from a tourist restaurant in Nagasaki, Japan. J Clin Microbiol 2005;43 (3):1093–8.
link1
[166]
Paranthaman K, Pringle E, Burgess A, Macdonald N, Sedgwick J. An unusual outbreak of norovirus associated with a Halloween-themed swimming pool party in England, 2016. Euro Surveill 2018;23(44):1700773.
link1
[167]
Podewils LJ, Zanardi Blevins L, Hagenbuch M, Itani D, Burns A, Otto C, et al. Outbreak of norovirus illness associated with a swimming pool. Epidemiol Infect 2007;135(5):827–33.
link1
[168]
Valcin R, Entringer M. Multi-jurisdictional norovirus outbreak at a swimming pool. Texas Public Health J 2014;66(3):15.
link1
[169]
Wade TJ, Augustine SAJ, Griffin SM, Sams EA, Oshima KH, Egorov AI, et al. Asymptomatic norovirus infection associated with swimming at a tropical beach: a prospective cohort study. PLoS ONE 2018;13(3):e0195056.
link1
[170]
Alsved M, Fraenkel CJ, Bohgard M, Widell A, Söderlund-Strand A, Lanbeck P, et al. Sources of airborne norovirus in hospital outbreaks. Clin Infect Dis 2020;70(10):2023–8.
link1
[171]
Zhang TL, Lu J, Ying L, Zhu XL, Zhao LH, Zhou MY, et al. An acute gastroenteritis outbreak caused by GII.P16–GII.2 norovirus associated with airborne transmission via the air conditioning unit in a kindergarten in Lianyungang, China. Int J Infect Dis 2017;65:81–4.
link1
[172]
Cheng HY, Hung MN, Chen WC, Lo YC, Su YS, Wei HY, et al. Ice-associated norovirus outbreak predominantly caused by GII.17 in Taiwan, 2015. BMC Public Health 2017;17(1):870.
link1
[173]
Ruan F, Tan AJ, Man TF, Li H, Mo YL, Lin YX, et al. Gastroenteritis outbreaks caused by norovirus genotype II.7 in a college in China (Zhuhai, Guangdong) in 2011. Foodborne Pathog Dis 2013;10(10):856–60.
link1
[174]
Guo XH, Kan Z, Liu BW, Li LL. A foodborne acute gastroenteritis outbreak caused by GII.P16–GII.2 norovirus in a boarding high school, Beijing, China: a case-control study. BMC Res Notes 2018;11(1):439.
link1
[175]
Shi C, Feng WH, Shi P, Ai J, Guan HX, Sha D, et al. An acute gastroenteritis outbreak caused by GII.17 norovirus in Jiangsu Province, China. Int J Infect Dis 2016;49:30–2.
link1
[176]
Qin M, Dong XG, Jing YY, Wei XX, Wang ZE, Feng HR, et al. A waterborne gastroenteritis outbreak caused by Norovirus GII.17 in a hotel, Hebei, China, December 2014. Food Environ Virol 2016;8(3):180–6.
[177]
Luo LF, Qiao K, Wang XG, Ding KY, Su HL, Li CZ, et al. Acute gastroenteritis outbreak caused by a GII.6 norovirus. World J Gastroenterol 2015;21 (17):5295–302.
link1
[178]
Chen D, Li Y, Lv J, Liu X, Gao P, Zhen G, et al. A foodborne outbreak of gastroenteritis caused by norovirus and Bacillus cereus at a university in the Shunyi District of Beijing, China 2018: a retrospective cohort study. BMC Infect Dis 2019;19(1):910.
link1
[179]
Isakbaeva ET, Widdowson MA, Beard RS, Bulens SN, Mullins J, Monroe SS, et al. Norovirus transmission on cruise ship. Emerg Infect Dis 2005;11 (1):154–8.
link1
[180]
Wu HM, Fornek M, Schwab KJ, Chapin AR, Gibson K, Schwab E, et al. A norovirus outbreak at a long-term-care facility: the role of environmental surface contamination. Infect Control Hosp Epidemiol 2005;26 (10):802–10.
link1
[181]
Riera-Montes M, Brus Sjölander K, Allestam G, Hallin E, Hedlund KO, Löfdahl M. Waterborne norovirus outbreak in a municipal drinking-water supply in Sweden. Epidemiol Infect 2011;139(12):1928–35.
link1
[182]
Purpari G, Giammanco GM, Ruggeri FM, Rotolo V, Costantino C, Macaluso G, et al. Surveillance of a municipal drinking-water supply after a norovirus outbreak in Italy. Int J Infect Dis 2012;16:e143.
link1
[183]
Maunula L, Klemola P, Kauppinen A, Söderberg K, Nguyen T, Pitkänen T, et al. Enteric viruses in a large waterborne outbreak of acute gastroenteritis in Finland. Food Environ Virol 2009;1(1):31–6.
link1
[184]
Cannon RO, Poliner JR, Hirschhorn RB, Rodeheaver DC, Silverman PR, Brown EA, et al. A multistate outbreak of Norwalk virus gastroenteritis associated with consumption of commercial ice. J Infect Dis 1991;164(5):860–3.
link1
[185]
Fell G, Boyens M, Baumgarte S. Tiefkühlfrüchte als Risikofaktor für Gastroenteritis-Ausbrüche durch Noroviren: Ergebnisse einer Ausbruchsuntersuchung im Sommer 2005 in Hamburg. Bundesgesundheitsbl 2007;50(2):230–6. German.
[186]
Braeye T, DE Schrijver K, Wollants E, van Ranst M, Verhaegen J. A large community outbreak of gastroenteritis associated with consumption of drinking water contaminated by river water, Belgium, 2010. Epidemiol Infect 2015;143(4):711–9.
[187]
Vivancos R, Keenan A, Sopwith W, Smith K, Quigley C, Mutton K, et al. Norovirus outbreak in a cruise ship sailing around the British Isles: investigation and multi-agency management of an international outbreak. J Infect 2010;60(6):478–85.
link1
[188]
Carling PC, Bruno-Murtha LA, Griffiths JK. Cruise ship environmental hygiene and the risk of norovirus infection outbreaks: an objective assessment of 56 vessels over 3 years. Clin Infect Dis 2009;49(9):1312–7.
link1
[189]
Verhoef L, Boxman IL, Duizer E, Rutjes SA, Vennema H, Friesema IHM, et al. Multiple exposures during a norovirus outbreak on a river-cruise sailing through Europe, 2006. Euro Surveill 2008;13(24):18899.
link1
[190]
Centers for Disease Control and Prevention (CDC). Norovirus outbreak in an elementary school—District of Columbia, February 2007. MMWR Morb Mortal Wkly Rep 2008;56(51–52):1340–3.
[191]
Cui C, Pan L, Wang Y, Xue C, Zhu W, Zhu L, et al. An outbreak of acute GII.17 norovirus gastroenteritis in a long-term care facility in China: the role of nursing assistants. J Infect Public Health 2017;10(6):725–9.
link1
[192]
Becker KM, Moe CL, Southwick KL, MacCormack JN. Transmission of Norwalk virus during a football game. N Engl J Med 2000;343(17):1223–7.
link1
[193]
Centers for Disease Control and Prevention (CDC). Multistate outbreak of norovirus gastroenteritis among attendees at a family reunion—Grant County, West Virginia, October 2006. MMWR Morb Mortal Wkly Rep 2007;56(27):673–8.
[194]
Li Y, Guo H, Xu Z, Zhou X, Zhang H, Zhang L, et al. An outbreak of norovirus gastroenteritis associated with a secondary water supply system in a factory in South China. BMC Public Health 2013;13(1):283.
link1
[195]
Zomer TP, De Jong B, Kühlmann-Berenzon S, Nyrén O, Svenungsson B, Hedlund KO, et al. A foodborne norovirus outbreak at a manufacturing company. Epidemiol Infect 2010;138(4):501–6.
link1
[196]
Boccia D, Tozzi AE, Cotter B, Rizzo C, Russo T, Buttinelli G, et al. Waterborne outbreak of Norwalk-like virus gastroenteritis at a tourist resort, Italy. Emerg Infect Dis 2002;8(6):563–8.
link1
[197]
Kappus KD, Marks JS, Holman RC, Bryant JK, Baker C, Gary GW, et al. An outbreak of Norwalk gastroenteritis associated with swimming in a pool and secondary person-to-person transmission. Am J Epidemiol 1982;116 (5):834–9.
link1
[198]
Kukkula M, Maunula L, Silvennoinen E, von Bonsdorff CH. Outbreak of viral gastroenteritis due to drinking water contaminated by Norwalk-like viruses. J Infect Dis 1999;180(6):1771–6.
link1
[199]
Anderson AD, Garrett VD, Sobel J, Monroe SS, Fankhauser RL, Schwab KJ, et al. Multistate outbreak of Norwalk-like virus gastroenteritis associated with a common caterer. Am J Epidemiol 2001;154(11):1013–9.
link1
[200]
Kaplan JE, Goodman RA, Schonberger LB, Lippy EC, Gary GW. Gastroenteritis due to Norwalk virus: an outbreak associated with a municipal water system. J Infect Dis 1982;146(2):190–7.
link1
[201]
Love SS, Jiang X, Barrett E, Farkas T, Kelly S. A large hotel outbreak of Norwalk-like virus gastroenteritis among three groups of guests and hotel employees in Virginia. Epidemiol Infect 2002;129(1):127–32.
link1
[202]
Peipins LA, Highfill KA, Barrett E, Monti MM, Hackler R, Huang P, et al. A Norwalk-like virus outbreak on the Appalachian Trail. J Environ Health 2002;64(9):18–23,32.
[203]
Kuusi M, Nuorti JP, Maunula L, Minh Tran NN, Ratia M, Karlsson J, et al. A prolonged outbreak of Norwalk-like calicivirus (NLV) gastroenteritis in a rehabilitation centre due to environmental contamination. Epidemiol Infect 2002;129(1):133–8.
link1
[204]
Lawson HW, Braun MM, Glass RI, Stine SE, Monroe SS, Atrash HK, et al. Waterborne outbreak of Norwalk virus gastroenteritis at a southwest US resort: role of geological formations in contamination of well water. Lancet 1991;337(8751):1200–4.
link1
[205]
Wilson R, Anderson LJ, Holman RC, Gary GW, Greenberg HB. Waterborne gastroenteritis due to the Norwalk agent: clinical and epidemiologic investigation. Am J Public Health 1982;72(1):72–4.
link1
[206]
Marks PJ, Vipond IB, Regan FM, Wedgwood K, Fey RE, Caul EO. A school outbreak of Norwalk-like virus: evidence for airborne transmission. Epidemiol Infect 2003;131(1):727–36.
link1
[207]
Carrique-Mas J, Andersson Y, Petersén B, Hedlund KO, Sjögren N, Giesecke J. A norwalk-like virus waterborne community outbreak in a Swedish village during peak holiday season. Epidemiol Infect 2003;131(1):737–44.
link1
[208]
Johansson PJH, Torvén M, Hammarlund AC, Björne U, Hedlund KO, Svensson L. Food-borne outbreak of gastroenteritis associated with genogroup I calicivirus. J Clin Microbiol 2002;40(3):794–8.
link1
[209]
Arness MK, Feighner BH, Canham ML, Taylor DN, Monroe SS, Cieslak TJ, et al. Norwalk-like viral gastroenteritis outbreak in U.S. Army trainees. Emerg Infect Dis 2000;6(2):204–7.
link1
[210]
Marks PJ, Vipond IB, Carlisle D, Deakin D, Fey RE, Caul EO. Evidence for airborne transmission of Norwalk-like virus (NLV) in a hotel restaurant. Epidemiol Infect 2000;124(3):481–7.
link1
[211]
Chover Lara JL, Pastor Vicente S, Roig Sena J, Roselló Pérez M, Salvo Samanes C, Castellanos Martínez I. Gastroenteritis outbreak associated with water consumption, possibly caused by Norwalk or Norwalk-like virus. Rev Esp Salud Publica 1995;69(2):243–54. Spanish.
[212]
Schets FM, van den Berg HHJL, Vennema H, Pelgrim MTM, Collé C, Rutjes SA, et al. Norovirus outbreak associated with swimming in a recreational lake not influenced by external human fecal sources in the Netherlands, August 2012. Int J Environ Res Public Health 2018;15(11):E2550.
link1
[213]
Kukkula M, Arstila P, Klossner ML, Maunula L, Bonsdorff CH, Jaatinen P. Waterborne outbreak of viral gastroenteritis. Scand J Infect Dis 1997;29 (4):415–8.
link1
[214]
Centers for Disease Control (CDC). Viral gastroenteritis—south Dakota and New Mexico. MMWR Morb Mortal Wkly Rep 1988;37(5):69–71.
[215]
Centers for Disease Control (CDC). Community outbreak of Norwalk gastroenteritis—Georgia. MMWR Morb Mortal Wkly Rep 1982;31(30):405–7.
link1
[216]
Centers for Disease Control (CDC). Gastroenteritis outbreaks on two Caribbean cruise ships. MMWR Morb Mortal Wkly Rep 1986;35(23):383–4.
[217]
Baron RC, Murphy FD, Greenberg HB, Davis CE, Bregman DJ, Gary GW, et al. Norwalk gastrointestinal illness: an outbreak associated with swimming in a recreational lake and secondary person-to-person transmission. Am J Epidemiol 1982;115(2):163–72.
link1
[218]
Warner RD, Carr RW, McCleskey FK, Johnson PC, Elmer LMG, Davison VE. A large nontypical outbreak of Norwalk virus. Gastroenteritis associated with exposing celery to nonpotable water and with Citrobacter freundii. Arch Intern Med 1991;151(12):2419–24.
link1
[219]
Liu B, Maywood P, Gupta L, Campbell B. An outbreak of Norwalk-like virus gastroenteritis in an aged-care residential hostel. N S W Public Health Bull 2003;14(6):105–9.
link1
[220]
Cheesbrough JS, Green J, Gallimore CI, Wright PA, Brown DW. Widespread environmental contamination with Norwalk-like viruses (NLV) detected in a prolonged hotel outbreak of gastroenteritis. Epidemiol Infect 2000;125 (1):93–8.
link1
[221]
Evans MR, Meldrum R, Lane W, Gardner D, Ribeiro CD, Gallimore CI, et al. An outbreak of viral gastroenteritis following environmental contamination at a concert hall. Epidemiol Infect 2002;129(2):355–60.
link1
[222]
Kobayashi S, Morishita T, Yamashita T, Sakae K, Nishio O, Miyake T, et al. A large outbreak of gastroenteritis associated with a small round structured virus among schoolchildren and teachers in Japan. Epidemiol Infect 1991;107 (1):81–6.
link1
[223]
Kilgore PE, Belay ED, Hamlin DM, Noel JS, Humphrey CD, Gary HE, et al. A university outbreak of gastroenteritis due to a small round-structured virus. Application of molecular diagnostics to identify the etiologic agent and patterns of transmission. J Infect Dis 1996;173(4):787–93.
link1
[224]
Gellert GA, Waterman SH, Ewert D, Oshiro L, Giles MP, Monroe SS, et al. An outbreak of acute gastroenteritis caused by a small round structured virus in a geriatric convalescent facility. Infect Control Hosp Epidemiol 1990;11 (9):459–64.
link1
[225]
Beller M, Ellis A, Lee SH, Drebot MA, Jenkerson SA, Funk E, et al. Outbreak of viral gastroenteritis due to a contaminated well. International consequences. JAMA 1997;278(7):563–8.
link1
[226]
Maurer AM, Stürchler D. A waterborne outbreak of small round structured virus, campylobacter and shigella co-infections in La Neuveville, Switzerland, 1998. Epidemiol Infect 2000;125(2):325–32.
link1
[227]
Schvoerer E, Bonnet F, Dubois V, Rogues AM, Gachie JP, Lafon ME, et al. A hospital outbreak of gastroenteritis possibly related to the contamination of tap water by a small round structured virus. J Hosp Infect 1999;43 (2):149–54.
link1
[228]
Brugha R, Vipond IB, Evans MR, Sandifer QD, Roberts RJ, Salmon RL, et al. A community outbreak of food-borne small round-structured virus gastroenteritis caused by a contaminated water supply. Epidemiol Infect 1999;122(1):145–54.
link1
[229]
Ho MS, Glass RI, Monroe SS, Madore HP, Stine S, Pinsky PF, et al. Viral gastroenteritis aboard a cruise ship. Lancet 1989;2(8669):961–5.
link1
[230]
McAnulty JM, Rubin GL, Carvan CT, Huntley EJ, Grohmann G, Hunter R. An outbreak of Norwalk-like gastroenteritis associated with contaminated drinking water at a caravan park. Aust J Public Health 1993;17(1):36–41.
link1
[231]
Chalmers JW, McMillan JH. An outbreak of viral gastroenteritis associated with adequately prepared oysters. Epidemiol Infect 1995;115(1):163–7.
link1
[232]
Chadwick PR, McCann R. Transmission of a small round structured virus by vomiting during a hospital outbreak of gastroenteritis. J Hosp Infect 1994;26 (4):251–9.
link1
[233]
Green J, Wright PA, Gallimore CI, Mitchell O, Morgan-Capner P, Brown DWG. The role of environmental contamination with small round structured viruses in a hospital outbreak investigated by reverse-transcriptase polymerase chain reaction assay. J Hosp Infect 1998;39(1):39–45.
link1
[234]
Iversen AM, Gill M, Bartlett CLR, Cubitt WD, McSwiggan DA. Two outbreaks of foodborne gastroenteritis caused by a small round structured virus: evidence of prolonged infectivity in a food handler. Lancet 1987;2(8558):556–8.
link1
[235]
Bergeisen GH, Hinds MW, Skaggs JW. A waterborne outbreak of hepatitis A in Meade County, Kentucky. Am J Public Health 1985;75(2):161–4.
link1
[236]
Bloch AB, Stramer SL, Smith JD, Margolis HS, Fields HA, McKinley TW, et al. Recovery of hepatitis A virus from a water supply responsible for a common source outbreak of hepatitis A. Am J Public Health 1990;80(4):428–30.
link1
[237]
Bryan JA, Lehmann JD, Setiady IF, Hatch MH. An outbreak of hepatitis-A associated with recreational lake water. Am J Epidemiol 1974;99(2):145–54.
link1
[238]
Divizia M, Gabrieli R, Donia D, Macaluso A, Bosch A, Guix S, et al. Waterborne gastroenteritis outbreak in Albania. Water Sci Technol 2004;50(1):57–61.
link1
[239]
Warburton ARE, Wreghitt TG, Rampling A, Buttery R, Ward KN, Perry KR, et al. Hepatitis A outbreak involving bread. Epidemiol Infect 1991;106 (1):199–202.
link1
[240]
Barrett CE, Pape BJ, Benedict KM, Foster MA, Roberts VA, Rotert K, et al. Impact of public health interventions on drinking water-associated outbreaks of hepatitis A—United States, 1971–2017. MMWR Morb Mortal Wkly Rep 2019;68(35):766–70.
link1
[241]
Mollers M, Boxman ILA, Vennema H, Slegers-Fitz-James IA, Brandwagt D, Friesema IH, et al. Successful use of advertisement pictures to assist recall in a food-borne hepatitis a outbreak in the Netherlands, 2017. Food Environ Virol 2018;10(3):272–7.
link1
[242]
Lucioni C, Cipriani V, Mazzi S, Panunzio M. Cost of an outbreak of hepatitis A in Puglia, Italy. Pharmacoeconomics 1998;13(2):257–66.
link1
[243]
Cooksley WGE. What did we learn from the Shanghai hepatitis A epidemic? J Viral Hepat 2000;7(Suppl 1):1–3.
link1
[244]
Xu YQ, Cui FQ, Zhuo JT, Zhang GM, Du JF, Den QY, et al. An outbreak of hepatitis A associated with a contaminated well in a middle school, Guangxi, China. Western Pac Surveill Response J 2012;3(4):44–7.
link1
[245]
Chironna M, Lopalco P, Prato R, Germinario C, Barbuti S, Quarto M. Outbreak of infection with hepatitis A virus (HAV) associated with a foodhandler and confirmed by sequence analysis reveals a new HAV genotype IB variant. J Clin Microbiol 2004;42(6):2825–8.
link1
[246]
Ruchusatsawat K, Wongpiyabovorn J, Kawidam C, Thiemsing L, Sangkitporn S, Yoshizaki S, et al. An outbreak of acute hepatitis caused by genotype IB hepatitis A viruses contaminating the water supply in Thailand. Intervirology 2016;59(4):197–203.
link1
[247]
Pal S, Juyal D, Sharma M, Kotian S, Negi V, Sharma N. An outbreak of hepatitis A virus among children in a flood rescue camp: a post-disaster catastrophe. Indian J Med Microbiol 2016;34(2):233–6.
link1
[248]
Hejkal T, Keswick B, Labelle R, Gerba C, Sanchez Y, Dreesman G, et al. Viruses in a community water supply associated with an outbreak of gastroenteritis and infectious hepatitis. J Am Water Resour Assoc 1982;74(6):318–21.
link1
[249]
De Medici D, Alfonsi V, Bruni R, Busani L, Ciccaglione AR, Di Pasquale S, et al. Hepatitis A outbreak in Italy associated with frozen berries: Dario De Medici. Eur J Public Health 2014;24(Suppl 2):cku165-041
link1
[250]
Bosch A, Sánchez G, Le Guyader F, Vanaclocha H, Haugarreau L, Pintó RM. Human enteric viruses in coquina clams associated with a large hepatitis A outbreak. Water Sci Technol 2001;43(12):61–5.
link1
[251]
De Serres G, Cromeans TL, Levesque B, Brassard N, Barthe C, Dionne M, et al. Molecular confirmation of hepatitis A virus from well water: epidemiology and public health implications. J Infect Dis 1999;179(1):37–43.
link1
[252]
Mahoney FJ, Farley TA, Kelso KY, Wilson SA, Horan JM, McFarland LM. An outbreak of hepatitis A associated with swimming in a public pool. J Infect Dis 1992;165(4):613–8.
link1
[253]
Tallis G, Gregory J. An outbreak of hepatitis A associated with a spa pool. Commun Dis Intell 1997;21(23):353–4.
link1
[254]
Shin E, Kim JS, Oh KH, Oh SS, Kwon M, Kim S, et al. A waterborne outbreak involving hepatitis A virus genotype IA at a residential facility in the Republic of Korea in 2015. J Clin Virol 2017;94:63–6.
link1
[255]
Bosch A, Lucena F, Diez JM, Gajardo R, Blasi M, Jofre J. Waterborne viruses associated with hepatitis outbreak. J Am Water Works Assn 1991;83(3):80–3.
link1
[256]
Kumar T, Shrivastava A, Kumar A, Khasnobis P, Narain JP, Laserson KF, et al. Hepatitis A outbreak associated with unsafe drinking water in a medical college student’s hostel, New Delhi, India, 2014. Int J Infect Dis 2016;45:442.
link1
[257]
Frank C, Walter J, Muehlen M, Jansen A, van Treeck U, Hauri AM, et al. Major outbreak of hepatitis A associated with orange juice among tourists, Egypt, 2004. Emerg Infect Dis 2007;13(1):156–8.
link1
[258]
Nordic Outbreak Investigation Team C. Joint analysis by the Nordic countries of a hepatitis A outbreak, October 2012 to June 2013: frozen strawberries suspected. Euro Surveill 2013;18(27):20520.
[259]
Rizzo C, Alfonsi V, Bruni R, Busani L, Ciccaglione A, De Medici D, et al.; Central Task Force on Hepatitis A. Ongoing outbreak of hepatitis A in Italy: preliminary report as of 31 May 2013. Euro Surveill 2013;18(27):20518.
[260]
Chi H, Haagsma EB, Riezebos-Brilman A, van den Berg AP, Metselaar HJ, de Knegt RJ. Hepatitis A related acute liver failure by consumption of contaminated food. J Clin Virol 2014;61(3):456–8.
link1
[261]
Collier MG, Khudyakov YE, Selvage D, Adams-Cameron M, Epson E, Cronquist A, et al.; Hepatitis A Outbreak Investigation Team. Outbreak of hepatitis A in the USA associated with frozen pomegranate arils imported from Turkey: an epidemiological case study. Lancet Infect Dis 2014;14(10):976–81.
link1
[262]
Belabbes EH, Bouguermouh A, Benatallah A, Illoul G. Epidemic non-A, non-B viral hepatitis in Algeria: strong evidence for its spreading by water. J Med Virol 1985;16(3):257–63.
link1
[263]
Brautbar N, Navizadeh N. Sewer workers: occupational risk for hepatitis C—report of two cases and review of literature. Arch Environ Health 1999;54 (5):328–30.
link1
[264]
Craun GF. Disease outbreaks caused by drinking water. J Water Pollut Control Fed 1979;51(6):1751–60.
link1
[265]
Ehresmann KR, Hedberg CW, Grimm MB, Norton CA, MacDonald KL, Osterholm MT. An outbreak of measles at an international sporting event with airborne transmission in a domed stadium. J Infect Dis 1995;171 (3):679–83.
link1
[266]
Goldstein DM, Hammon WM, Viets HR. An outbreak of polioencephalitis among Navy Cadets, possibly food borne. J Am Med Assoc 1946;131 (7):569–73.
link1
[267]
Drenchen A, Bert M. A gastroenteritis illness outbreak associated with swimming in campground lake. J Environ Health 1994;57:7.
link1
[268]
Acheson ED. Encephalomyelitis associated with poliomyelitis virus; an outbreak in a nurses’ home. Lancet 1954;267(6847):1044–8.
link1
[269]
Kandun IN, Samaan G, Harun S, Purba WH, Sariwati E, Septiawati C, et al. Chicken faeces garden fertilizer: possible source of human avian influenza H5N1 infection. Zoonoses Public Health 2010;57(4):285–90.
link1
[270]
Soule H, Gratacap-Cavallier B, Genoulaz O, Potelon JL, Francois P, Zmirou D, et al. Role of drinking water in rotavirus spread: a case-control study in the Isere region, France. Med Mal Infect 1999;29(1):13–8.
link1
[271]
Chitambar SD, Lahon A, Tatte VS, Maniya NH, Tambe GU, Khatri KI, et al. Occurrence of group B rotavirus infections in the outbreaks of acute gastroenteritis from western India. Indian J Med Res 2011;134(3): 399–400.
link1
[272]
Hopkins RS, Gaspard GB, Williams FP Jr, Karlin RJ, Cukor G, Blacklow NR. A community waterborne gastroenteritis outbreak: evidence for rotavirus as the agent. Am J Public Health 1984;74(3):263–5.
link1
[273]
Brown DWG, Campbell L, Tomkins DS, Hambling MH. School outbreak of gastroenteritis due to atypical rotavirus. Lancet 1989;2(8665):737–8.
link1
[274]
Turner M, Istre GR, Beauchamp H, Baum M, Arnold S. Community outbreak of adenovirus type 7a infections associated with a swimming pool. South Med J 1987;80(6):712–5.
link1
[275]
Russell Kevin L, Broderick Michael P, Franklin Suzanne E, Blyn Lawrence B, Freed Nikki E, Moradi E, et al. Transmission dynamics and prospective environmental sampling of adenovirus in a military recruit setting. J Infect Dis 2006;194(7):877–85.
link1
[276]
Cui X, Wen L, Wu Z, Liu N, Yang C, Liu W, et al. Human adenovirus type 7 infection associated with severe and fatal acute lower respiratory illness and nosocomial transmission. J Clin Microbiol 2015;53(2):746–9.
link1
[277]
D’Angelo LJ, Hierholzer JC, Keenlyside RA, Anderson LJ, Martone WJ. Pharyngoconjunctival fever caused by adenovirus type 4: report of a swimming pool-related outbreak with recovery of virus from pool water. J Infect Dis 1979;140(1):42–7.
link1
[278]
Li J, Lu X, Sun Y, Lin C, Li F, Yang Y, et al. A swimming pool-associated outbreak of pharyngoconjunctival fever caused by human adenovirus type 4 in Beijing. China. Int J Infect Dis 2018;75:89–91.
link1
[279]
Sung H. An adenovirus outbreak associated with a swimming facility. SM Trop Med J 2016;1(2):1–3.
link1
[280]
Hein A. North Dakota woman dies from hantavirus after possible contact with rodent droppings [Internet]. Los Angeles: FOX News Network, LLC; 2018 Aug 27 [cited 2020 Jul 15]. Available from: https://www.foxnews.com/ health/north-dakota-woman-dies-from-hantavirus-after-possible-contactwith-rodent-droppings.
link1
[281]
Man contracts hantavirus after staying in cabins at California park, family says [Internet]. Los Angeles: FOX News Network, LLC; 2017 Jul 18 [cited 2020 Jul 15]. Available from: https://www.foxnews.com/health/man-contractshantavirus-after-staying-in-cabins-at-california-park-family-says.
link1
[282]
Rat infection: North Wales owner catches hantavirus. London: BBC News; 2013.
[283]
Preidt R. 8 people infected in rare U.S. outbreak of rat virus [Internet]. Washington, DC: CBS News; 2017 Jan 23 [cited 2020 Jul 15]. Available from: https://www.cbsnews.com/news/rats-seoul-virus-people-infected-inrare-u-s-outbreak/.
link1
[284]
Farber M. 9 family members infected with coronavirus after sharing hot pot meal. Los Angeles: FOX News Network, LLC; 2020.
link1
[285]
Middle East respiratory syndrome coronavirus (MERS-CoV)—the United Arab Emirates. Geneva: World Health Organization; 2019.
[286]
Zumla A, Hui DS, Perlman S. Middle East respiratory syndrome. Lancet 2015;386(9997):995–1007.
link1
[287]
Kida K, Matsuoka Y, Shimoda T, Matsuoka H, Yamada H, Saito T, et al. A case of cat-to-human transmission of severe fever with thrombocytopenia syndrome virus. Jpn J Infect Dis 2019;72(5):356–8.
link1
[288]
Hein A. Mom’s herpes warning after son contracts virus, possibly putting unborn baby at risk [Internet]. Los Angeles: FOX News Network, LLC; 2019 Aug 1 [cited 2020 Jul 15]. Available from: https://www.foxnews.com/ health/moms-herpes-warning-son-virus-unborn-baby-risk.
link1
[289]
How humanity unleashed a flood of new diseases [Internet]. New York: The New York Times; 2020 Jun 17 [Cited 2020 Jul 15]. Available from: https:// www.nytimes.com/2020/06/17/magazine/animal-disease-covid.html.
link1
[290]
Christian MD, Loutfy M, McDonald LC, Martinez KF, Ofner M, Wong T, et al; SARS Investigation Team. Possible SARS coronavirus transmission during cardiopulmonary resuscitation. Emerg Infect Dis 2004;10(2):287–93.
link1
[291]
Yu ITS, Li Y, Wong TW, Tam W, Chan AT, Lee JHW, et al. Evidence of airborne transmission of the severe acute respiratory syndrome virus. N Engl J Med 2004;350(17):1731–9.
link1
[292]
Booth TF, Kournikakis B, Bastien N, Ho J, Kobasa D, Stadnyk L, et al. Detection of airborne severe acute respiratory syndrome (SARS) coronavirus and environmental contamination in SARS outbreak units. J Infect Dis 2005;191 (9):1472–7.
link1
[293]
Li Y, Duan S, Yu IT, Wong TW. Multi-zone modeling of probable SARS virus transmission by airflow between flats in Block E, Amoy Gardens. Indoor Air 2005;15(2):96–111.
link1
[294]
Reisen WK, Takahashi RM, Carroll BD, Quiring R. Delinquent mortgages, neglected swimming pools, and West Nile virus, California. Emerg Infect Dis 2008;14(11):1747–9.
link1
[295]
Greenbaum A, Quinn C, Bailer J, Su S, Havers F, Durand LO, et al. Investigation of an outbreak of variant influenza A (H3N2) virus infection associated with an agricultural fair—Ohio, August 2012. J Infect Dis 2015;212 (10):1592–9.
link1
[296]
Moser MR, Bender TR, Margolis HS, Noble GR, Kendal AP, Ritter DG. An outbreak of influenza aboard a commercial airliner. Am J Epidemiol 1979;110 (1):1–6.
link1
[297]
Han K, Zhu XP, He F, Liu LG, Zhang LJ, Ma HL, et al. Lack of airborne transmission during outbreak of pandemic (H1N1) 2009 among tour group members, China, June 2009. Emerg Infect Dis 2009;15(10):1578–81.
link1
[298]
Koopmans M, Wilbrink B, Conyn M, Natrop G, van der Nat H, Vennema H, et al. Transmission of H7N7 avian influenza A virus to human beings during a large outbreak in commercial poultry farms in the Netherlands. Lancet 2004;363(9409):587–93.
link1
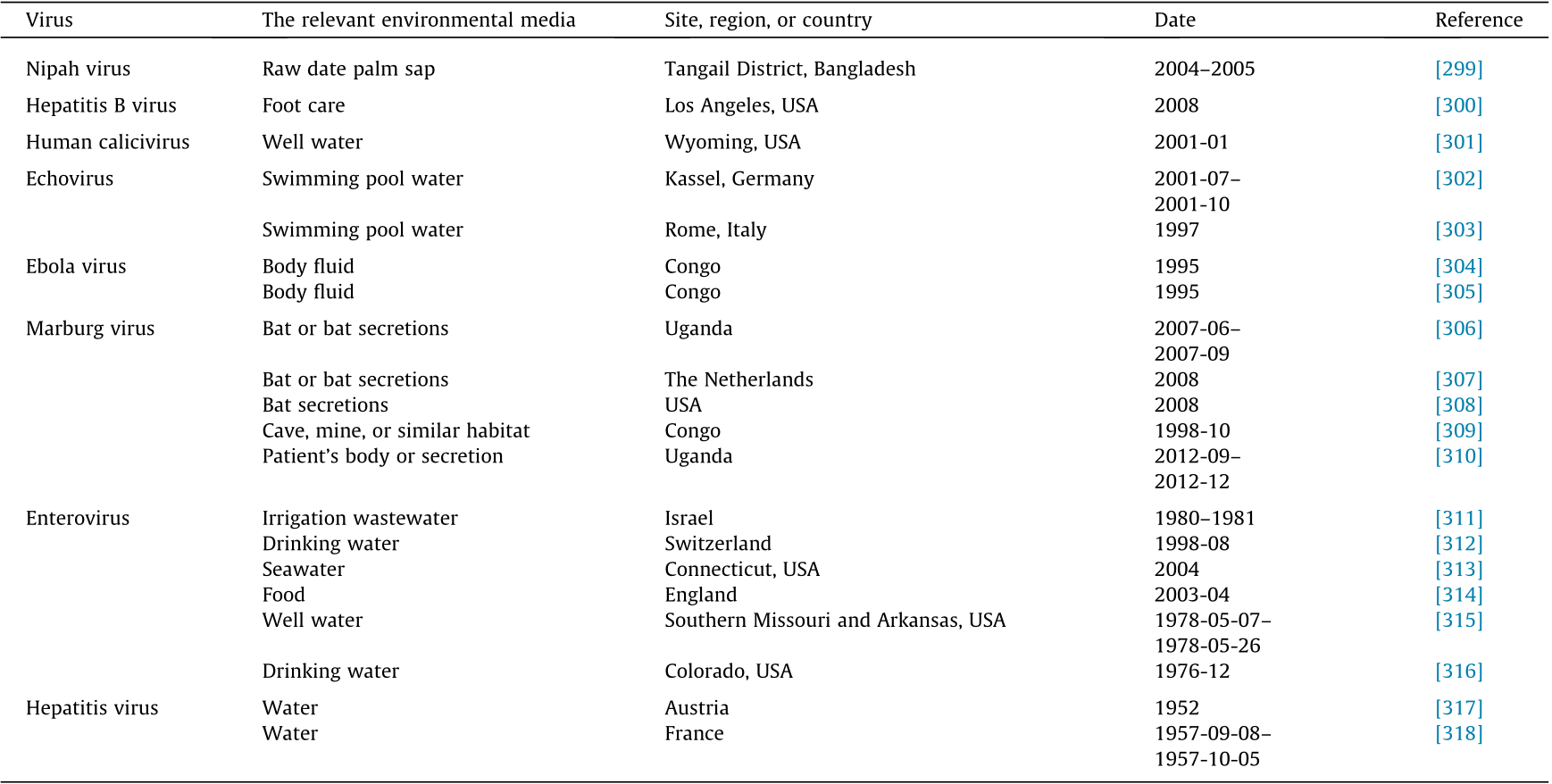
[299]
Luby SP, Rahman M, Hossain MJ, Blum LS, Husain MM, Gurley E, et al. Foodborne transmission of Nipah virus, Bangladesh. Emerg Infect Dis 2006;12(12):1888–94.
link1
[300]
Wise ME, Marquez P, Sharapov U, Hathaway S, Katz K, Tolan S, et al. Outbreak of acute hepatitis B virus infections associated with podiatric care at a psychiatric long-term care facility. Am J Infect Control 2012;40 (1):16–21.
link1
[301]
Parshionikar SU, Willian-True S, Fout GS, Robbins DE, Seys SA, Cassady JD, et al. Waterborne outbreak of gastroenteritis associated with a norovirus. Appl Environ Microbiol 2003;69(9):5263–8.
link1
[302]
Hauri AM, Schimmelpfennig M, Walter-Domes M, Letz A, Diedrich S, LopezPila J, et al. An outbreak of viral meningitis associated with a public swimming pond. Epidemiol Infect 2005;133(2):291–8.
link1
[303]
Faustini A, Fano V, Muscillo M, Zaniratti S, La Rosa G, Tribuzi L, et al. An outbreak of aseptic meningitis due to echovirus 30 associated with attending school and swimming in pools. Int J Infect Dis 2006;10(4):291–7.
link1
[304]
Dowell SF, Mukunu R, Ksiazek TG, Khan AS, Rollin PE, Peters CJ, et al.; Commission de Lutte contre les Epidémies à Kikwit. Transmission of Ebola hemorrhagic fever: a study of risk factors in family members, Kikwit, Democratic Republic of the Congo, 1995. J Infect Dis 1999;179 (Suppl 1):S87– 91.
[305]
Khan AS, Tshioko FK, Heymann DL, Le Guenno B, Nabeth P, Kerstiëns B, et al.; Commission de Lutte contre les Epidémies à Kikwit. The reemergence of Ebola hemorrhagic fever, Democratic Republic of the Congo, 1995. J Infect Dis 1999;179(Suppl 1):S76–86.
[306]
Adjemian J, Farnon EC, Tschioko F, Wamala JF, Byaruhanga E, Bwire GS, et al. Outbreak of Marburg hemorrhagic fever among miners in Kamwenge and Ibanda Districts, Uganda, 2007. J Infect Dis 2011;204(Suppl 3):S796–9.
link1
[307]
Timen A, Koopmans MPG, Vossen ACTM, van Doornum GJJ, Günther S, van den Berkmortel F, et al. Response to imported case of Marburg hemorrhagic fever, the Netherland. Emerg Infect Dis 2009;15(8):1171–5.
link1
[308]
Centers for Disease Control and Prevention (CDC). Imported case of Marburg hemorrhagic fever—Colorado, 2008. MMWR Morb Mortal Wkly Rep 2009;58 (49):1377–81.
[309]
Bausch DG, Nichol ST, Muyembe-Tamfum JJ, Borchert M, Rollin PE, Sleurs H, et al.; International Scientific and Technical Committee for Marburg Hemorrhagic Fever Control in the Democratic Republic of the Congo. Marburg hemorrhagic fever associated with multiple genetic lineages of virus. N Engl J Med 2006;355(9):909–19.
link1
[310]
Mbonye A, Wamala J, Winyi-Kaboyo, Tugumizemo V, Aceng J, Makumbi I. Repeated outbreaks of viral hemorrhagic fevers in Uganda. Afr Health Sci 2012;12(4):579–83.
link1
[311]
Fattal B, Margalith M, Shuval HI, Wax Y, Morag A. Viral antibodies in agricultural populations exposed to aerosols from wastewater irrigation during a viral disease outbreak. Am J Epidemiol 1987;125(5):899–906.
link1
[312]
Häfliger D, Hübner P, Lüthy J. Outbreak of viral gastroenteritis due to sewage-contaminated drinking water. Int J Food Microbiol 2000;54(1–2): 123–6.
link1
[313]
Begier EM, Oberste MS, Landry ML, Brennan T, Mlynarski D, Mshar PA, et al. An outbreak of concurrent echovirus 30 and coxsackievirus A1 infections associated with sea swimming among a group of travelers to Mexico. Clin Infect Dis 2008;47(5):616–23.
link1
[314]
Gallimore CI, Pipkin C, Shrimpton H, Green AD, Pickford Y, McCartney C, et al. Detection of multiple enteric virus strains within a foodborne outbreak of gastroenteritis: an indication of the source of contamination. Epidemiol Infect 2005;133(1):41–7.
link1
[315]
Centers for Disease Control and Prevention (CDC). Gastroenteritis associated with a sewage leak—Missouri, Arkansas. MMWR Morb Mortal Wkly Rep 1978;27(22):183–4.
[316]
Morens DM, Zweighaft RM, Vernon TM, Gary GW, Eslien JJ, Wood BT, et al. A waterborne outbreak of gastroenteritis with secondary person-to-person spread. Association with a viral agent. Lancet 1979;1(8123):964–6.
link1
[317]
Peczenik A, Duttweiler DW, Moser RH. An apparently water-borne outbreak of infectious hepatitis. Am J Public Health Nations Health 1956;46 (8):1008–17.
link1
[318]
Randel HW, Bovee CW. Infectious hepatitis: a waterborne outbreak at an air base in France. Am J Public Health Nations Health 1962;52(9):1483–500.
link1
[319]
Tian H, Lei Y, Liu Y, Yang DJ, Zhuo Z. Etiological survey of acute gastroenteritis caused by norovirus. J Environ Health 2014;31(09):796–8.
link1
[320]
Rulli MC, Santini M, Hayman DTS, D’Odorico P. The nexus between forest fragmentation in Africa and Ebola virus disease outbreaks. Sci Rep 2017;7 (1):41613.
link1
[321]
Walsh MG, Mor SM, Maity H, Hossain S. Forest loss shapes the landscape suitability of Kyasanur Forest disease in the biodiversity hotspots of the Western Ghats. India. Int J Epidemiol 2019;48(6):1804–14.
link1
[322]
MacDonald AJ, Larsen AE, Plantinga AJ. Missing the people for the trees: identifying coupled natural–human system feedbacks driving the ecology of Lyme disease. J Appl Ecol 2019;56(2):354–64.
link1
[323]
Plowright RK, Eby P, Hudson PJ, Smith IL, Westcott D, Bryden WL, et al. Ecological dynamics of emerging bat virus spillover. Proc R Soc B 1798;2015:282.
link1
[324]
Ji W, Wang W, Zhao X, Zai J, Li X. Cross-species transmission of the newly identified coronavirus 2019-nCoV. J Med Virol 2020;92(4):433–40.
link1
[325]
Li X, Song Y, Wong G, Cui J. Bat origin of a new human coronavirus: there and back again. Sci China Life Sci 2020;63(3):461–2.
link1
[326]
Salata C, Calistri A, Parolin C, Palù G. Coronaviruses: a paradigm of new emerging zoonotic diseases. Pathog Dis 2019;77(9):ftaa006.
link1
[327]
Woo PCY, Lau SKP, Lam CSF, Lau CCY, Tsang AKL, Lau JHN, et al. Discovery of seven novel Mammalian and avian coronaviruses in the genus deltacoronavirus supports bat coronaviruses as the gene source of alphacoronavirus and betacoronavirus and avian coronaviruses as the gene source of gammacoronavirus and deltacoronavirus. J Virol 2012;86 (7):3995–4008.
link1
[328]
Hu B, Zeng LP, Yang XL, Ge XY, Zhang W, Li B, et al. Discovery of a rich gene pool of bat SARS-related coronaviruses provides new insights into the origin of SARS coronavirus. PLoS Pathog 2017;13(11):e1006698.
link1
[329]
Cui J, Li F, Shi ZL. Origin and evolution of pathogenic coronaviruses. Nat Rev Microbiol 2019;17(3):181–92.
link1
[330]
World Health Organization. Consensus document on the epidemiology of severe acute respiratory syndrome (SARS). Geneva: World Health Organization; 2013.
link1
[331]
Dhama K, Khan S, Tiwari R, Sircar S, Bhat S, Malik YS, et al. Coronavirus disease 2019-COVID-19. Clin Microbiol Rev 2020;33(4). e00028-20.
link1
[332]
Dhama K, Pawaiya R, Chakraborty S, Tiwari R, Saminathan M, Verma A. Coronavirus infection in Equines: a review. Asian J Anim Vet Adv 2014;9 (3):164–76.
link1
[333]
Dhama K, Singh SD, Barathidasan R, Desingu PA, Chakraborty S, Tiwari R, et al. Emergence of avian infectious bronchitis virus and its variants need better diagnosis, prevention and control strategies: a global perspective. Pak J Biol Sci 2014;17(6):751–67.
link1
[334]
Monchatre-Leroy E, Boué F, Boucher JM, Renault C, Moutou F, Ar Gouilh M, et al. Identification of a and b coronavirus in wildlife species in France: bats, rodents, rabbits, and hedgehogs. Viruses 2017;9(12):364.
link1
[335]
Malik YS, Sircar S, Bhat S, Vinodhkumar OR, Tiwari R, Sah R, et al. Emerging coronavirus disease (COVID-19), a pandemic public health emergency with animal linkages: current status update. Preprints 202003.0343.v1.
[336]
Xu Y. Genetic diversity and potential recombination between ferret coronaviruses from European and American lineages. J Infect 2020;80 (3):350–71.
link1
[337]
Lidgerding B, Hetrick F. Fish cell line: persistent infection with a coronavirus. In Vitro 1983;19(3 Pt II):286.
[338]
Sano T, Yamaki T, Fukuda H. A novel carp coronavirus, characterization and pathogenicity. In: International Fish Health Conference, Vancouver; 1988 Jul 19–21; Vancouver, BC, Canada; 1988.
[339]
Miyazaki T, Okamoto H, Kageyama T, Kobayashi T. Viremia-associated anaaki-byo, a new viral disease in color carp Cyprinus carpio in Japan. Dis Aquat Organ 2000;39(3):183–92.
link1




















 京公网安备 11010502051620号
京公网安备 11010502051620号




